Main Page: Difference between revisions
mNo edit summary |
No edit summary |
||
| (46 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<html> | |||
<iframe src="https://glioblastomatreatments.wiki/mm.html" | |||
style="width: 100%; height: 620px; border: 0;"> | |||
</iframe> | |||
<BR/><BR/> | |||
<iframe src="https://glioblastomatreatments.wiki/mm2.html" | |||
style="width: 100%; height: 620px; border: 0;"> | |||
</iframe> | |||
</html> | |||
[[File:Metformin.png|thumb|Metformin chat with Oncologist]] | |||
<div class="mw-collapsible mw-collapsed"> | |||
Since my own diagnosis of glioblastoma (GBM) in 1995 at age 50, I have spent | |||
considerable time researching treatment options, and the following discussion | |||
summarizes what I have learned. Most of the information is from medical journals and | |||
the proceedings of major cancer conferences. Some information has been contributed by | |||
others to various online brain tumor patient support groups, which I have followed up on, | |||
and some is from direct communications with various physicians conducting the | |||
treatments that are described. References are presented at the end for those who would | |||
like their physicians to take this information seriously. Although this discussion is | |||
intended to be primarily descriptive of the recent development of new treatment options, | |||
it is motivated by my belief that single-agent treatment protocols are unlikely to be | |||
successful, and patients are best served if they utilize multiple treatment modalities, and | |||
go beyond the “certified” treatments that too often are the only treatment options offered. | |||
<div class="mw-collapsible-content"> | |||
A more extensive account of my philosophy of treatment, and the reasons for it, are | |||
provided in my (2002) book, Surviving "Terminal" Cancer: Clinical Trials, Drug | |||
Cocktails, and Other Treatments Your Doctor Won't Tell You About. | |||
Currently, it is available only at Amazon.com, where reviews of the book also are | |||
available. | |||
When I began my search for effective treatments, the available options offered little | |||
chance for surviving my diagnosis. The standard treatment included surgery, radiation, | |||
and nitrosourea-based chemotherapy, either BCNU alone or CCNU combined with | |||
procarbazine and vincristine (known as the PCV combination). While this treatment has | |||
helped a small minority of people, its 5-year survival rate has been only 2-5%. Median | |||
survival has been about a year, which is 2-3 months longer than for patients receiving | |||
radiation alone without chemotherapy. Fortunately, as will be discussed in the next | |||
section, the past ten years has produced a new “gold standard” of treatment for newly | |||
diagnosed patients: the combination of radiation with a new chemotherapy agent, | |||
temozolomide (trade name Temodar in the USA and Temodal elsewhere in the world). | |||
While this new standard appears to produce a notable improvement over previous | |||
treatments, it still falls far short of being effective for the great majority of patients. | |||
Also available now are three other treatments that have FDA approval for tumors that | |||
have recurred or have progressed after initial treatment: Gliadel, Avastin, and an | |||
electrical field therapy named Optune (formerly known as NovoTTF). All of these are | |||
considered standard of care for recurrent tumors (which is important for insurance | |||
reasons), and can legally also be used for newly diagnosed patients as well. Each will be | |||
discussed later in this article. | |||
There are three general premises to the approach to treatment that will be described. The | |||
first is borrowed from the treatment approach that has evolved in the treatment of AIDS. | |||
Both viruses and cancer cells have unstable genetic structures susceptible to mutations. | |||
This implies that the dynamics of evolution will create new forms that are resistant to | |||
whatever the treatment may be. However, if several different treatments are used | |||
simultaneously (instead of sequentially, which is typically the case), any given mutation | |||
has a smaller chance of being successful. A mathematical model instantiating these | |||
assumptions has recently been developed and has been shown to describe the pattern of | |||
tumor growth for melanoma (1). | |||
The second premise is that cancer treatments of all sorts are probabilistic in their effects. | |||
None work for everyone, in part because any given cancer diagnosis is an amalgam of | |||
different genetic defects that respond in different ways to any given treatment agent. This | |||
is especially true for glioblastomas, which have a multiplicity of genetic aberrations that | |||
vary widely across individuals and sometimes even within the same tumor of a given | |||
individual. As a result it is common that any given "effective" treatment agent will | |||
benefit only a minority of patients, often in the range of 10-35%, but do little if anything | |||
for the majority. The result is that the chances of finding an effective treatment increase | |||
the more different treatment agents that are utilized. Probabilistic effects can and do | |||
summate. | |||
An important implication of the genetic diversity of GBM tumors is that tests of | |||
treatment agents presented individually will often fail, not because they lack | |||
effectiveness, but because they target only one or sometimes two growth pathways, | |||
leaving other growth pathways to be upregulated to maintain the growth of the tumor. | |||
Thus, even at the level of clinical trials, tests of individual treatment agents in isolation | |||
may be a misguided strategy. A drug that fails in isolation might in fact be effective when | |||
combined with other drugs that target the additional alternative growth pathways. | |||
A third general principle is that any successful treatment needs to be systemic in nature | |||
because it is impossible to identify all of the extensions of the tumor into normal tissue. | |||
Moreover, cancer cells are typically evident in locations in the brain distant from the | |||
main tumor, indicating that metastases within the brain can occur, although the great | |||
majority of tumor recurrences are within or proximal to the original tumor site. Localized | |||
treatments such as radiosurgery may be beneficial in terms of buying time, but they are | |||
unlikely to provide a cure, except in cases when the tumor is detected early and is very | |||
small. Even if the localized treatment eradicates 99% of the tumor, the small amount of | |||
residual tumor will expand geometrically, eventually causing significant clinical | |||
problems. | |||
Until the development of immunological treatments in just the last few years, which will | |||
be discussed in a later section, the only systemic treatment available has been cytotoxic | |||
chemotherapy, which historically has been ineffective except for a small percentage of | |||
patients. An important issue, therefore, is whether chemotherapy can be made to work | |||
substantially better than it typically does. Agents that facilitate or augment its effects are | |||
critically important. As will be seen, a number of older drugs developed for other | |||
purposes have been shown in laboratory studies to be effective against cancer, often with | |||
minimal toxicity. The availability of these treatments raises the possibility that some | |||
combination of these new agents can be packaged that provide effective treatment based | |||
on several different independent principles. Thus, the AIDS-type of combination | |||
approach is now a genuine possibility whereas it would not have been fifteen years ago. | |||
Because many of these relatively nontoxic new agents were developed for purposes other | |||
than cancer, or for different kinds of cancer, their utilization in the treatment of | |||
glioblastomas is "off-label", with the result that many oncologists have been hesitant to | |||
prescribe them. Thus, patients themselves need to become familiar with these new agents | |||
and the evidence available regarding their clinical effectiveness. It is possible, although | |||
by no means proven, that some combination of these newly repurposed agents offers the | |||
best possibility for survival. | |||
Patients may or may not learn about the treatments that will be described from their | |||
physicians. To appreciate why, it is important to understand how American medicine has | |||
been institutionalized. For most medical problems there is an accepted standard of what | |||
is the best available treatment. Ideally, such treatments are based on phase III clinical | |||
trials in which patients are randomly assigned to receive the new treatment or some type | |||
of control condition. Treatments that have been studied only in nonrandomized phase II | |||
trials will rarely be offered as a treatment option, even if the accepted "best available | |||
treatment" is generally ineffective. What happens instead is that patients are encouraged | |||
to participate in clinical trials. The problem with this approach is that most medical | |||
centers offer few options for an individual patient. Thus, even though a given trial for a | |||
new treatment may seem very promising, patients can participate only if that trial is | |||
offered by their medical facility. Yet more problematic is that clinical trials with new | |||
treatment agents almost always initially study that agent in isolation, usually with | |||
patients with recurrent tumors who have the worst prognoses. For newly diagnosed | |||
patients this is at best a last resort. What is needed instead is access to the most | |||
promising new treatments, in the optimum combinations, at the time of initial diagnosis. | |||
In the discussion to follow, it is important to distinguish between treatment options at the | |||
time of initial diagnosis versus those when the tumor either did not respond to the initial | |||
treatment or responded for a period of time and then recurred. Different measures of | |||
treatment efficacy are often used for the two situations, which sometimes makes | |||
treatment information obtained in one setting difficult to apply to the other. The | |||
recurrent tumor situation is also complicated by the fact that resistance to the initial | |||
treatment may or may not generalize to new treatments given at recurrence. | |||
The Importance of Brain Tumor Centers | |||
When someone is diagnosed with a brain tumor they are faced with a situation about | |||
which they know very little, but nevertheless must develop a treatment plan very quickly, | |||
because GBMs grow very rapidly if left untreated. The first step, if possible, is to have as | |||
much of the tumor removed as possible, because various data show substantially | |||
increased survival times for those with complete resections, relative to those who have | |||
incomplete resections or only biopsies. Accordingly, it is best that patients seek treatment | |||
at a major brain tumor center because neurosurgeons there will have performed many | |||
more tumor removals than general neurosurgeons that typically work in the community | |||
setting. This is especially important in recent times, as surgical techniques have become | |||
increasingly more sophisticated and utilize procedures that community treatment centers | |||
do not have the resources to perform. I know of numerous cases in which a local | |||
neurosurgeon has told the patient the tumor is inoperable, only to have the same tumor | |||
completely removed at a major brain tumor center. | |||
An additional advantage of utilizing a major brain tumor center is that they are better | |||
equipped to do genetic analyses of tumor tissue, which are increasingly important in | |||
guiding treatment decisions. Moreover, they provide a gateway into clinical trials. | |||
</div> | |||
</div> | |||
==The Importance of Brain Tumor Centers== | |||
When someone is diagnosed with a brain tumor they are faced with a situation about | |||
which they know very little, but nevertheless must develop a treatment plan very quickly, | |||
because GBMs grow very rapidly if left untreated. The first step, if possible, is to have as | |||
much of the tumor removed as possible, because various data show substantially | |||
increased survival times for those with complete resections, relative to those who have | |||
incomplete resections or only biopsies. Accordingly, it is best that patients seek treatment | |||
at a major brain tumor center because neurosurgeons there will have performed many | |||
more tumor removals than general neurosurgeons that typically work in the community | |||
setting. This is especially important in recent times, as surgical techniques have become | |||
increasingly more sophisticated and utilize procedures that community treatment centers | |||
do not have the resources to perform. I know of numerous cases in which a local | |||
neurosurgeon has told the patient the tumor is inoperable, only to have the same tumor | |||
completely removed at a major brain tumor center. | |||
An additional advantage of utilizing a major brain tumor center is that they are better | |||
equipped to do genetic analyses of tumor tissue, which are increasingly important in | |||
guiding treatment decisions. Moreover, they provide a gateway into clinical trials. | |||
==The Standard of Care for Initial Treatment== | |||
===Glioblastoma=== | |||
Although chemotherapy has a long history of being ineffective as a treatment for | |||
glioblastoma, a large randomized European-Canadian clinical trial (EORTC trial | |||
26981/22981) has shown clear benefits of adding the new chemotherapy agent, | |||
temozolomide (trade name Temodar in the USA, Temodal elsewhere in the world) to the | |||
standard radiation treatment (2). This treatment, followed by 6 or more monthly cycles of | |||
temozolomide, has become known as the “Stupp protocol” after Roger Stupp, the Swiss | |||
oncologist who led the trial. In this trial, one group of patients received radiation alone; | |||
the other group received radiation plus Temodar, first at low daily dosages during the six | |||
weeks of radiation, followed by the standard schedule of higher-dose Temodar for days | |||
1-5 out of every 28-day cycle. Median survival was 14.6 months, compared to a median | |||
survival of 12 months for patients receiving radiation only, a difference that was | |||
statistically significant. More impressive was the difference in two-year survival rate, | |||
which was 27% for the patients receiving temodar but 10% for those receiving only | |||
radiation. Longer-term follow-up has indicated that the benefit of temozolomide (TMZ) | |||
persists at least up to five years: The difference in survival rates between the two | |||
treatment conditions was 16.4% vs. 4.4% after three years, 12.1% vs. 3.0% after four years, | |||
and 9.8% vs. 1.9% after five years (3). As a result of these findings, the protocol of TMZ | |||
presented during radiation is now recognized as the "gold standard" of treatment. Note, | |||
however, that all of these numbers are somewhat inflated because patients over the age of | |||
70 were excluded from the trial. | |||
In July of 2016, the National Comprehensive Cancer Network (NCCN) recommended | |||
Optune as a category 1 treatment for newly diagnosed glioblastoma in combination with | |||
the standard temozolomide-based chemotherapy (see press release here). This rating | |||
indicates a uniform consensus by the NCCN that this treatment is appropriate. As the | |||
NCCN is recognized as setting the standards for cancer treatment in the USA and in other | |||
countries abroad which follow its guidelines, Optune in combination with standard | |||
chemotherapy following radiation could now be considered to be a new standard of care | |||
for newly diagnosed glioblastoma. See more detailed information on Optune in Chapter | |||
3. | |||
Research summarized here: https://virtualtrials.org/optune/NVCR_Clinical_Evidence_Flipbook_9.5.23.pdf | |||
=== Cancer Stem Cells (CSCs) in Glioblastoma: Challenges with Standard of Care (SOC) === | |||
==== What Are Cancer Stem Cells? ==== | |||
Cancer stem cells (CSCs) are a small subpopulation of cells within tumors that possess capabilities similar to those of normal stem cells, such as self-renewal and differentiation. In the context of glioblastoma, these cells are often referred to as glioma stem cells (GSCs). They are believed to be crucial drivers of tumor growth, resistance to treatment, and recurrence. | |||
==== Standard of Care for Glioblastoma ==== | |||
The current standard of care for glioblastoma typically includes surgical resection followed by radiation therapy and chemotherapy with temozolomide. While these treatments can initially reduce tumor size and manage symptoms, they do not effectively target GSCs, which can survive treatments and cause tumor recurrence. | |||
==== Why Does SOC Fail to Prevent Recurrence? ==== | |||
* '''Resistance to Treatment:''' GSCs are highly resistant to chemotherapy and radiation. They have efficient DNA repair mechanisms and can remain dormant during treatment, evading the effects of SOC that target rapidly dividing cells. | |||
* '''Microenvironment Protection:''' GSCs reside in protective niches within the tumor microenvironment that shield them from the effects of SOC. These niches provide support and maintain the stem-like qualities of GSCs, promoting their ability to regenerate the tumor. | |||
* '''Tumor Regeneration:''' After treatment, surviving GSCs can regenerate the tumor, often leading to a recurrence that is more aggressive and resistant to further treatment. This cycle is a significant challenge in the management of glioblastoma. | |||
==== Research and Future Directions ==== | |||
Understanding the biology of GSCs has led to the exploration of targeted therapies aimed at these cells. Strategies include developing drugs that specifically target the molecular pathways essential for GSC survival and proliferation, disrupting the tumor microenvironment, and using immunotherapy to enhance the body's natural defenses against these cells. | |||
==== Conclusion ==== | |||
The recurrence of glioblastoma post-SOC is largely due to the presence and behavior of GSCs. Efforts to improve glioblastoma treatment outcomes must focus on effectively targeting these cells. Ongoing research into the molecular and environmental underpinnings of GSCs holds promise for developing more effective therapies that can prevent recurrence and extend patient survival. | |||
<div style="background-color: #ffffcc; padding: 10px; margin-top: 10px; border-left: 6px solid #ffeb3b;"> | |||
'''Note:''' While alternatives to SOC are not proven to always work, exploring such options is crucial because without trying different approaches, recurrence is almost guaranteed. | |||
</div> | |||
==== Alternative Therapies Targeting GSCs ==== | |||
Various alternative therapies have been explored for their potential to target glioma stem cells (GSCs) in glioblastoma. These are considered experimental and have been primarily studied in preclinical trials or ongoing research settings: | |||
* '''[[Curcumin]]''': This compound, derived from turmeric, has anti-inflammatory properties and has been studied for its potential to disrupt pathways involved in cancer stem cell growth and survival. | |||
* '''[[Resveratrol]]''': Found in grapes and berries, resveratrol has been researched for its ability to inhibit the growth of cancer stem cells and induce apoptosis in various cancer cell models, including glioblastoma. | |||
* '''[[Sulforaphane]]''': A compound in cruciferous vegetables like broccoli, sulforaphane targets cellular processes that are critical for cancer cell growth and survival, impacting cancer stem cells. | |||
* '''[[CBD]]''': Research suggests that CBD may affect glioblastoma by targeting the stem-like properties of GSCs, potentially reducing their ability to contribute to tumor growth. | |||
* '''[[Metformin]]''': While primarily used for diabetes management, metformin has shown potential in preclinical studies for its anti-cancer effects and ability to target cancer stem cells in glioblastoma. | |||
* '''[[Disulfiram]]''': Traditionally used for treating alcohol dependency, disulfiram has been studied for its capacity to target cancer stem cells in glioblastoma, particularly when used in combination with copper. | |||
* '''[[Parthenolide]]''': This compound, from the herb feverfew, is being researched for its ability to induce oxidative stress and apoptosis in glioblastoma stem cells. | |||
* '''[[:Category:Repurposed Drugs|Repurposed Drugs]]''': Drugs approved for other conditions, such as antidepressants or antipsychotics, have been explored for their ability to interfere with signaling pathways critical for the maintenance of cancer stem cells and tumor resistance. | |||
These therapies are still under investigation for their effectiveness and safety in treating glioblastoma and are generally considered for clinical trial settings. Patients should consult with healthcare professionals and consider clinical trials where these treatments are being tested. | |||
===Anaplastic astrocytoma=== | |||
Though the “Stupp protocol” of combined temoradiation (concomitant radiation and | |||
temozolomide chemotherapy) followed by monthly cycles of temozolomide has been | |||
routinely applied to anaplastic astrocytoma patients, prospective confirmation of this use | |||
in this patient population has awaited results of the “CATNON” randomized phase 3 trial | |||
for 1p/19q non-codeleted grade 3 gliomas. Results of the interim analysis for this trial | |||
were first released for the ASCO 2016 annual meeting. Between 2007 and 2015, 748 | |||
patients were randomized to receive either i) radiation alone, ii) radiation with | |||
concomitant temozolomide, iii) radiation followed by 12 adjuvant monthly cycles of | |||
temozolomide, or iv) radiation with temozolomide both concurrently and with follow-up | |||
monthly cycles. At the time of the interim analysis (October 2015), significant | |||
progression-free and overall survival benefit was found with adjuvant temozolomide | |||
treatment (arms iii and iv). Median progression-free survival was 19 months in arms i | |||
and ii (not receiving adjuvant temozolomide) versus 42.8 months (receiving adjuvant | |||
temozolomide). 5-year survival rate was 44.1% and 55.9% in arms i and ii versus iii and | |||
iv. Median survival was not yet reached for arms iii and iv. | |||
This analysis did not address the benefit of temozolomide concurrent with radiation, a | |||
question that will be answered with further follow-up, and studies assessing the impact of | |||
IDH1 mutation and MGMT methylation were still ongoing. | |||
===Determining who will benefit=== | |||
A two-year survival rate of less than 30% obviously cannot be considered an effective | |||
treatment, as the great majority of patients receiving the treatment obtain at best a minor | |||
benefit, accompanied with significant side effects (although Temodar is much better | |||
tolerated than previous chemotherapy treatments, especially with respect to the | |||
cumulative toxicity to the bone marrow). This raises the issues of how to determine who | |||
will benefit from the treatment, and, most importantly, how to improve the treatment | |||
outcomes. | |||
One approach to determining whether an individual patient will benefit from | |||
chemotherapy is simply to try 1-2 rounds to see if there is any tumor regression. The | |||
debilitating effects of chemotherapy typically occur in later rounds, at which point there | |||
is a cumulative decline in blood counts. The extreme nausea and vomiting associated | |||
with chemotherapy in the mind of the lay public is now almost completely preventable by | |||
anti-nausea agents, including Zofran (ondansetron), Kytril (granisetron) and Emend. | |||
(aprepitant). Marijuana also can be very effective in controlling such effects, and recent | |||
research has suggested that it has anti-cancer properties in its own right. Thus, for those | |||
patients who are relatively robust after surgery and radiation, some amount of | |||
chemotherapy experimentation should be possible without major difficulties. | |||
An alternative way to ascertain the value of chemotherapy for an individual patient is the | |||
use of chemosensitivity testing for the various drugs that are possible treatments. Such | |||
testing typically requires a live sample of the tumor and thus must be planned in advance | |||
of surgery. Culturing the live cells is often problematic, but a number of private | |||
companies across the country offer this service. Costs range from $1000-$2500, | |||
depending on the scope of drugs that are tested. Such testing is controversial, in part | |||
because the cell population evolves during the process of culturing, which results in cells | |||
possibly different in important ways from the original tumor sample. Nevertheless, | |||
recent evidence has shown that chemosensitivity testing can enhance treatment | |||
effectiveness for a variety of different types of cancer, including a recent Japanese study | |||
using chemosensitivity testing with glioblastoma patients (4). However, this study did not | |||
involve cell culturing but direct tests of chemosensitivity for cells harvested at the time of | |||
surgery. In general, when chemosensitivity testing indicates an agent has no effect on a | |||
patient's tumor the drug is unlikely to have any clinical benefit. On the other hand, tests | |||
indicating that a tumor culture is sensitive to a particular agent do not guarantee clinical | |||
effectiveness, but increase the likelihood that the agent will be beneficial. | |||
=== The Role of MGMT === | |||
A significant advance in determining which patients will benefit from Temodar was | |||
reported by the same research group that reported the definitive trial combining Temodar | |||
with radiation. Tumor specimens from the patients in that trial were tested for the level of | |||
activation of a specific gene involved in resistance to alkylating chemotherapy (which | |||
includes temozolomide and the nitrosoureas, BCNU, CCNU, and ACNU). | |||
[[MGMT| full text]] | |||
===Dexamethasone=== | |||
Most glioma patients will be exposed to dexamethasone (Decadron) at some point, as this | |||
corticosteroid is the first-line treatment to control cerebral edema caused by the leaky | |||
tumor blood vessels. Many also require dexamethasone during radiotherapy, and | |||
perhaps beyond this time if substantial tumor remains post-resection. Dexamethasone is | |||
an analog to the body’s own cortisol, but is about 25 times more potent. Though often | |||
necessary, dexamethasone comes with a long list of adverse potential side effects with | |||
prolonged use, including muscle weakness, bone loss, steroid-induced diabetes, | |||
immunosuppression, weight gain, and psychological effects. | |||
New evidence also shows an association between dexamethasone use and reduced | |||
survival time in glioblastoma. This evidence has to be weighed against the fact that | |||
uncontrolled cerebral edema can be fatal in itself, and that dexamethasone is often | |||
required for its control. However, the attempt should always be made to use | |||
dexamethasone at the lowest effective dose, and to taper its use after control of edema is | |||
achieved, under a physician’s guidance. | |||
In a retrospective study of 622 glioblastoma patients treated at Memorial Sloan Kettering | |||
Cancer Center, multivariate regression analysis showed an independent negative | |||
association of steroid use at the start of radiotherapy with survival (324). A similar | |||
negative association with survival outcomes was found in patients in the pivotal phase 3 | |||
trial that led to temozolomide being approved for glioblastoma in 2005, and for a cohort | |||
of 832 glioblastoma patients enrolled in the German Glioma Network. | |||
Follow up studies in mice helped elucidate these retrospective clinical observations. In a | |||
genetically engineered PDGFB-driven glioblastoma mouse model, dexamethasone alone | |||
had no effect on survival, but pretreatment with dexamethasone for 3 days prior to a | |||
single dose of 10 Gy radiation negatively impacted the efficacy of radiation. This negative | |||
impact of dexamethasone on radiation efficacy was even more dramatic with multiple | |||
doses of dexamethasone given before 5 treatments with 2 Gy radiation, which more | |||
closely mimics what GBM patients are exposed to. In contrast, an antibody against | |||
VEGF, which could be considered a murine surrogate for Avastin, did not interfere with | |||
the efficacy of radiation. | |||
In vivo mechanistic examination revealed that dexamethasone may interfere with | |||
radiation by slowing proliferation, leading to a higher number of cells in the more | |||
radioresistant G1 phase of the cell cycle, and fewer cells in the more radiosensitive G2/M | |||
phase. This finding has far-reaching implications about the potential interference by | |||
drugs with cytostatic mechanisms of action on the efficacy of radiation therapy. | |||
The authors conclude by suggesting that antibodies against VEGF, most notably | |||
bevacizumab (Avastin), could be used as an alternative anti-edema drug during radiation | |||
in place of steroids. However, this use has to be weighed in importance against the | |||
exclusion from certain promising clinical trials due to prior use of Avastin being an | |||
exclusion criteria in some of these trials. | |||
=== Radiation === | |||
====The Role of Radiation==== | |||
For many years the only treatment (other than surgery) offered to patients with | |||
glioblastomas was radiation, due to radiation being the only treatment found to improve | |||
survival time in randomized clinical trials. This continued to be the case in Europe until | |||
the last decade, but in this country chemotherapy (usually BCNU) gradually came to be | |||
accepted as a useful additional treatment component despite the absence of definitive | |||
evidence from clinical trials. Part of the reason for this acceptance of chemotherapy has | |||
been that very few patients receiving only radiation survive longer than two years (3- | |||
10%), compared to 15-25% of patients also receiving chemotherapy. | |||
The initial approach to using radiation to treat gliomas was whole-head radiation, but this | |||
was abandoned because of the substantial neurological deficits that resulted, sometimes | |||
appearing a considerable time after treatment. Current clinical practice uses a more | |||
focused radiation field that includes only 2-3 cm beyond the periphery of the tumor site. | |||
Because of the potential for radiation necrosis, the current level of radiation that is | |||
considered safe is limited to 55-60 Gy. Even at this level, significant deficits may occur, | |||
often appearing several years after treatment. The most common causes of these deficits | |||
are damage to the myelin of the large white fibers, which are the main transmitters of | |||
information between different centers of the brain, and damage to the small blood | |||
vessels, which results in an inadequate blood supply to the brain and also increases the | |||
likelihood of strokes. An additional risk, not yet proven clinically because of the typical | |||
short survival times of glioblastoma patients, is the growth of secondary tumors due to | |||
the radiation damage to the DNA. However, experimental work with animal models has | |||
supported the reality of this risk (208). Three-year-old normal rhesus monkeys were | |||
�given whole brain radiation using a protocol similar to the common human radiation | |||
protocol and then followed for 2-9 years thereafter. A startling 82% of the monkeys | |||
developed glioblastoma tumors during that follow-up period. It is currently unclear to | |||
what degree a similar risk occurs for human patients who are long-term survivors. | |||
The major additional use of radiation in the treatment of gliomas has been localized | |||
radiation to the tumor field, after the external-beam radiation treatment is finished (or | |||
sometimes concurrently), either by use of implanted radiation seeds (typically radioactive | |||
iodine), a procedure known as brachytherapy, the use of radiosurgery (including gamma | |||
knife), or by the insertion into the tumor cavity of an inflatable balloon containing | |||
radioactive fluid (gliasite). Previous editions of this treatment summary devoted | |||
considerable discussion to these treatments. However, these treatments now are used | |||
much less frequently. Two different randomized trials of brachytherapy failed to show a | |||
statistically significant survival benefit even though the procedure causes considerable | |||
toxicity in terms of radiation necrosis (209). A recent randomized study of radiosurgery | |||
(210) similarly failed to show a benefit. Gliasite has yet to be studied in a randomized | |||
trial. | |||
The usual interpretation of the failure to find a benefit in the randomized trials is that the | |||
initial studies indicating a survival benefit (usually increasing survival time about a year) | |||
involved a highly selected patient population, who otherwise had a good prognosis | |||
regardless of whether they received the procedure. However, selection bias seems not to | |||
account for all of the benefits of the procedure. For example, the use of gliasite for | |||
recurrent GBM tumors produced a median survival time of 36 weeks (211), which | |||
compares favorably with a median survival time of only 28 weeks when gliadel wafers | |||
were implanted for recurrent tumors, even though eligibility criteria were similar for the | |||
two procedures. Moreover, when patients receiving gliasite as part of the initial | |||
treatment (212) were partitioned according to according to established prognostic | |||
variables, and each partition was compared to its appropriate historical control, survival | |||
time was greater for patients receiving gliasite in each of the separate partitions. | |||
Perhaps the best results reported involving radiation boosts comes from the combination | |||
of permanent radioactive iodine seeds with gliadel (212). Median survival for patients | |||
with recurrent glioblastomas was 69 weeks, although accompanied by considerable brain | |||
necrosis. The use of gliadel alone in the same treatment center, by comparison, produced | |||
a median survival time of 28 weeks, while the use of the radiation seeds alone produced a | |||
median survival of 47 weeks. | |||
Impressive results have also been obtained with the addition of fractionated radiosurgery | |||
to the standard Stupp protocol for newly diagnosed patients (213). For 36 GBM patients | |||
median survival (from diagnosis) was 28 months and two-year survival was 57%. Median | |||
progression-free survival (from study entry) for the GBM patients was 10 months. | |||
�The foregoing results suggest that supplementary radiation procedures do provide some | |||
benefit, but it is important to appreciate that all only a portion of patients will be eligible | |||
for such treatment. Radiation necrosis caused by the treatment must be considered as | |||
well. | |||
====Hyberbaric oxygen and other radiosensitizers==== | |||
A potentially important modification of the standard radiation protocols involves the use | |||
of hyperbaric oxygen prior to each radiation session. In a study conducted in Japan (214), | |||
57 high-grade glioma patients received the standard radiation protocol with the addition | |||
of hyperbaric oxygen 15 minutes prior to each radiation session. Four rounds of | |||
chemotherapy were also administered, the first during the radiation period of treatment. | |||
For the 39 glioblastoma patients, the median survival time was 17 months, with a very | |||
high rate of tumor regression. For the 18 patients with anaplastic astrocytoma, median | |||
survival was 113 months. Two-year survival was reported separately for recursive | |||
partioning categories I-IV and V-VI, the latter including only glioblastoma patients. For | |||
categories I- IV, two-year survival was 50%; for categories V and VI, two-year survival | |||
was 38%. | |||
A long-standing goal of radiation oncology has been to find a radiation sensitizer that | |||
does not increase toxicity to normal tissue. One of the most promising advances toward | |||
this goal was reported at the 2011 ASCO meeting (215). A new drug derived from the | |||
taxane family, with the name OPAXIO, was combined with the standard Temodar + | |||
radiation protocol during the radiation phase of the treatment. The response rate for 25 | |||
patients (17 GBM) was 45% with 27% having a complete response. With a median | |||
follow-up of 22 months, median progression-free survival was 14.9 month (13.5 months | |||
for GBM patients). Median overall survival had not been reached at the time of the | |||
report. Note that the median PFS for the standard treatment without OPAXIO is 6.9 | |||
months. | |||
====Proton radiation therapy==== | |||
{{#ask: [[Has treatment name::Proton Beam Therapy (PBT)]] | |||
|?Has common side effects=Common Side Effects | |||
|?Has OS without=Overall Survival without PBT | |||
|?Has OS with=Overall Survival with PBT | |||
|?Has PFS without=Progression-Free Survival without PBT | |||
|?Has PFS with=Progression-Free Survival with PBT | |||
|?Has Usefulness Rating=Usefulness Rating | |||
|?Has Toxicity Level=toxicity_level | |||
|?Has Toxicity Explanation=Toxicity Explanation | |||
|format=table | |||
|limit=1 | |||
}} | |||
An alternative to the standard X-ray radiation is the use of proton beams, although only a | |||
few treatment centers have the required equipment. To date, there has been no | |||
meaningful comparison of the efficacy of proton-beam radiation and the normal | |||
procedure. However, one recent study in Japan did report unusually positive results | |||
when the two forms of radiation were combined, the standard procedure in the morning, | |||
and the proton-beam radiation in the afternoon (216). Also used was ACNU, a chemical | |||
cousin of BCNU and CCNU. Median survival for 20 patients was 21.6 month, with -1- | |||
year and 2-year progression-free rates of 45% and 16%. However, there were six cases of | |||
radiation necrosis that required surgery, indicating a considerably higher toxicity than | |||
normally occurs with the standard radiation procedure. | |||
====Gamma Knife Radiosurgery (GKRS) for GBM==== | |||
{{#ask: [[Has treatment name::Gamma Knife Radiosurgery (GKRS) for GBM]] | |||
|?Has common side effects=Common Side Effects | |||
|?Has OS without=Overall Survival without GKRS | |||
|?Has OS with=Overall Survival with GKRS | |||
|?Has PFS without=Progression-Free Survival without GKRS | |||
|?Has PFS with=Progression-Free Survival with GKRS | |||
|?Has Usefulness Rating=Usefulness Rating | |||
|?Has Toxicity Level=toxicity_level | |||
|?Has Toxicity Explanation=Toxicity Explanation | |||
|format=table | |||
|limit=1 | |||
}} | |||
The Gamma Knife radiosurgery (GKRS) for glioblastoma (GBM) showcases a potential treatment path with a lower toxicity profile, according to recent studies. This method, particularly through fractionated sessions using the Gamma Knife ICON, maintains progression-free and overall survival rates comparable to conventional treatments. The advantage lies in its safety and practicality for specific GBM patients, highlighting an approach that balances efficacy with reduced side effects. For detailed insights, refer to the study in BMC Cancer [here](https://bmccancer.biomedcentral.com/articles/10.1186/s12885-022-10162-w). | |||
====Radiation via Monoclonal Antibodies==== | |||
{{#ask: [[Has treatment name::Radiation via Monoclonal Antibodies]] | |||
|?Has common side effects=Common Side Effects | |||
|?Has OS without=Overall Survival without | |||
|?Has OS with=Overall Survival with | |||
|?Has PFS without=Progression-Free Survival without | |||
|?Has PFS with=Progression-Free Survival with | |||
|?Has Usefulness Rating=Usefulness Rating | |||
|?Has Toxicity Level=toxicity_level | |||
|?Has Toxicity Explanation=Toxicity Explanation | |||
|format=table | |||
|limit=1 | |||
}} | |||
An alternative for providing a radiation boost beyond the standard external field | |||
radiation involves attaching radioactive iodine-131 to a monoclonal antibody that targets | |||
a specific antigen, tenascin, which occurs on almost all high-grade glioma tumors and not | |||
on normal brain cells. The monoclonal antibodies are infused directly into the tumor | |||
cavity over a period of several days, and reportedly produces much less radiation necrosis | |||
than either brachytherapy or radiosurgery. The median survival time from a phase 2 | |||
clinical trial of this treatment for recurrent GBM tumors was 56 weeks (217). In the first | |||
study that reported using this approach as initial treatment (218) patients received the | |||
monoclonal antibodies, followed by the standard external-beam radiation and then a year | |||
of chemotherapy. Of 33 patients, only one required re-operation for necrotic tissue caused | |||
by the radiation. Median survival time was 79 weeks for the patients with glioblastoma | |||
(27 of 33 of total patients) and 87 weeks for all patients. Estimated two-year survival rate | |||
for GBM patients was 35%. A subsequent report of the results for an expanded number | |||
of patients indicated a mean progression-free survival of 17.2 months, compared to 4-10 | |||
months for other treatment procedures (219). Median overall survival measured from the | |||
time of diagnosis was 24.9 months. At the present time, however, only one treatment | |||
center (Duke University) has used this procedure. A multi-center clinical trial was | |||
planned, but the company sponsoring the trial apparently has shelved those plans for the | |||
indefinite future. | |||
A second type of monoclonal antibody treatment, developed at Hahneman University | |||
Medical School in Philadelphia, targets the epidermal growth factor receptor, which is | |||
overexpressed in the majority of GBM tumors (220) For patients who received the MAB | |||
treatment in combination with standard radiation, median survival time was 14.5 months; | |||
For patients who received the same protocol but with the addition of temodar, median | |||
survival was 20.4 months. | |||
A third type of monoclonal antibody, named Cotara, is designed to bind with proteins that | |||
are exposed only when cells are dying, with the result that adjacent living tumor cells are | |||
radiated by the radiation load carried by the monoclonal antibody. This rationale is based | |||
on the fact that that centers of GBM tumors have a large amount of necrosis. This | |||
approach has been under development by Peregrine Pharmaceuticals, a small biotech | |||
with limited funding. Recently they reported the long-term results from 28 recurrent | |||
GBM patients studied over a nine-year period (221). Seven of the 28 patients survived | |||
more than one year, while 3 of the 28 survived longer than five years (2 more than 9 | |||
years). Median survival was 38 weeks. | |||
==Strategies for improving the Standard of Care== | |||
===Combatting chemoresistance=== | |||
There are several ways that cancer cells evade being killed by cytotoxic chemotherapy. | |||
Already mentioned is that the damage inflicted by the chemotherapy is quickly repaired | |||
before actually killing the cell (due to the activity of the MGMT repair enzyme). A second | |||
source of resistance is that the chemo agent is extruded from the cancer before the next | |||
cell division (chemotherapy typically affects only those cells in the process of dividing). A | |||
third way is that the chemo agent doesn’t penetrate the blood-brain barrier. While | |||
Temodar is generally believed to cross the blood-brain-barrier effectively, empirical | |||
studies of its concentration within the tumor tissue have shown that its penetration is | |||
incomplete. | |||
A major source of chemo-resistance for many types of cancer comes from glycoprotein | |||
transport systems (technically called ABC transporters) that extrude the chemotherapy | |||
agent before it has the chance to kill the cell. This is important because chemotherapy is | |||
effective only when cells are dividing, and only a fraction of the cell population is dividing | |||
at any given time. The longer the chemotherapy remains in the cell, the more likely it will | |||
be there at the time of cell division. If extrusion of the chemotherapy drug could be | |||
inhibited, chemotherapy should in principle become more effective. Calcium channel | |||
blockers, which include commonly used medications for hypertension such as | |||
verapamil, have thus been studied for that purpose (11). | |||
Unfortunately, these agents have potent effects on the cardiovascular system, so that | |||
dosages sufficiently high to produce clinical benefits usually have not been achievable. | |||
However, a recent study (12) did report a substantial clinical benefit for patients with | |||
breast cancer with a relatively low dosage (240 mg/day). An earlier randomized trial with | |||
advanced lung cancer (13) also demonstrated a significant benefit of verapamil, using a | |||
dose of 480 mg/day, both in terms of frequency of tumor regression and survival time. In | |||
addition, the combination of verapamil with tamoxifen (which itself blocks the extrusion | |||
by a somewhat different mechanism) may possibly increase the clinical benefit (14). In | |||
laboratory studies, the calcium channel blockers nicardipine and nimodipine (15, 16) | |||
have also been shown to effectively increase chemotherapy effectiveness, and may have | |||
direct effects on tumor growth themselves. Quinine derivatives such as quinidine and | |||
chloroquine also inhibit the extrusion pump. Among the strongest inhibitors of the | |||
extrusion pump is a common drug used in the treatment of alcoholism, Antabuse, also | |||
known as disulfiram (17,18). Yet another class of drugs that keep the chemo inside for | |||
longer time periods are proton pump inhibitors used for acid reflux (e.g., Prilosec) (19). | |||
One approach to blocking the glycoprotein pump without the high toxic doses is to | |||
combine several agents together, using lower doses of each individual agent, as combining | |||
different agents has been shown to be synergistic in laboratory studies (20). | |||
The most promising clinical results for combatting chemo-resistance has come from the | |||
addition of chloroquine, an old anti-malaria drug, to the traditional chemotherapy | |||
agent, BCNU. See Chapter 5, Chloroquine section for further details. | |||
Disruption of the blood-brain-barrier (BBB) is also potentially very important and has | |||
been extensively investigated. The issue is complicated by the fact that tumor tissue | |||
already has a substantially disrupted BBB (which is the basis of using contrast agents to | |||
identify the tumor). However, this disruption is incomplete, so any chemotherapy agent | |||
that does not cross the intact BBB will not contact all portions of the tumor. Various | |||
ways of disrupting the BBB have been studied, but none has been generally successful, | |||
primarily because of their systemic side effects. Recently, however, the common erectile | |||
dysfunction drugs (Viagra, Levitra, Cialis) have been discovered to disrupt the BBB in | |||
laboratory animals. In a rat brain tumor model, the addition of Viagra or Levitra to a | |||
common chemotherapy agent, Adriamycin, substantially improved survival time (26). | |||
===Optimizing the Schedule of Chemotherapy=== | |||
The standard schedule for using full-dose Temodar is days 1-5 out of every 28-day cycle. | |||
The large phase 3 EORTC-NCIC study (2005) also added daily Temodar during radiation | |||
at a lower dosage, followed by the standard five-day schedule after radiation was | |||
completed. But there has never been a persuasive rationale for why this standard schedule | |||
should be preferred over various alternatives. | |||
In addition to the standard schedule, three other schedules have been studied: (1) a | |||
“metronomic” low-dose daily schedule; (2) an alternating week schedule; (3) a “dose- | |||
intense” schedule in which Temodar is used on days 1-21 of every 28-day cycle. While it | |||
is possible to compare the outcomes of these different studies across different clinical | |||
trials, only a few studies have compared the different schedules within the same clinical | |||
trial. | |||
�In one single-center randomized trial with newly diagnosed patients, the alternating week | |||
schedule of 150 mg/m2 on days 1-7 and 15-21 was compared with the metronomic | |||
schedule of 50 mg/m2 daily (29). Patients completing 6 cycles of adjuvant Temodar were | |||
switched to maintenace therapy with 13-cis retinoic acid (aka Accutane). One-year | |||
survival rates were 80% vs. 69%, and two-year survival rates 35% vs. 28%, both favoring | |||
the alternating week schedule. However, neither difference was statistically significant. | |||
Median survival times for the alternating week and metronomic schedules were 17.1 vs. | |||
15.1 months. | |||
A second very large randomized trial compared the standard 5-day schedule with a dose- | |||
intense schedule (75-100 mg/mz2 on days 1-21). The rationale of the dose-intense schedule | |||
was that it would better deplete the MGMT enzyme (30). Median PFS favored the | |||
dose-dense arm (6.7 months vs. 5.5 months from the time of study randomization, | |||
p=0.06), while median overall survival favored the standard schedule (16.6 vs. 14.9 | |||
months from randomization). While neither difference was considered statistically | |||
significant, the dose-intense schedule had substantially more toxicity and hence cannot be | |||
recommended. | |||
In a more recent retrospective study (313), 40 patients undergoing the standard 5-day | |||
temozolomide schedule and 30 patients undergoing a metronomic schedule (75 mg/m2) | |||
were included in the final analysis. The metronomic temozolomide schedule led to | |||
statistically significant increases in both progression-free survival and overall survival, | |||
and in both univariate and multivariate analysis. Even more importantly, this study found | |||
that the benefit of the metronomic schedule mainly occurs for those patients with EGFR | |||
overexpression (EGFR protein expression in over 30% of tumor cells), or EGFR gene | |||
amplification. Median overall survival for patients with EGFR overexpression treated with | |||
metronomic temozolomide was 34 months, compared to 12 months with standard | |||
schedule. EGFR overexpressing patients treated with metronomic temozolomide had | |||
highly statistically significantly improved progression-free survival and overall survival | |||
compared to all other groups (the other groups being EGFR overexpressing treated with | |||
standard schedule, and EGFR non-overexpressing treated with either schedule). | |||
The investigators furthermore analysed tumor tissue samples from patients who | |||
underwent repeat resection at the time of recurrence. Interestingly, they found that | |||
samples from EGFR overexpressing tumors treated with metronomic temozolomide had | |||
significantly fewer cells positive for NF-kB/p65 (a promoter of cell proliferation and | |||
survival) compared with untreated tumors from the same patients at the time of | |||
diagnosis. No such change was observed between the primary and recurrent EGFR | |||
overexpressing tumors from patients treated with the standard schedule. Recurrent | |||
EGFR amplified tumors treated with the metronomic schedule showed fewer EGFR | |||
amplified cells and weaker EGFR staining at the time of recurrence compared with the | |||
primary tumor. No such difference was observed in EGFR amplified tumors treated with | |||
�the standard schedule. The authors draw the conclusion that this metronomic schedule | |||
impairs survival of EGFR expressing GBM cells more effectively than the standard | |||
schedule. These findings will hopefully lead to testing in prospective clinical trials. A | |||
major caveat when reviewing this study is that there is no explanation for why some of the | |||
patients were selected for the higher dose metronomic schedule rather than the standard | |||
schedule and it’s possible that these patients were healthier at baseline and that selection | |||
bias contributed to the different outcomes. | |||
The lowest Temodar dose in metronomic chemotherapy reported to date was presented to | |||
newly diagnosed glioblastoma patients (44). After completion of standard radiation | |||
treatment, continuous daily doses of temozolomide approximately 1/10 of the typically | |||
used full dose were used in combination with Vioxx (aka rofecoxib, a discontinued COX-2 | |||
inhibitor which was later replaced by celecoxib in studies by this group). Median | |||
progression-free survival was 8 months and overall survival for 13 patients was 16 | |||
months, with minimal toxicity. A second retrospective study (45) from the same medical | |||
group compared the very low-dose schedule (20 mg/m2) with a more typical metronomic | |||
dosage (50 mg/meter-squared), although only 17 patients and six patients were included | |||
in the former and latter groups. Also included were patients who received only radiation. | |||
Median survival was 17 months and 21 months, respectively, for the two metronomic | |||
chemotherapy groups vs. 9 months for the radiation-only patients. | |||
Although clinicians will likely resist any alternative to the standard temozolomide | |||
schedule for newly diagnosed patients outside of clinical trials, a medium-dose | |||
metronomic schedule is worthy of consideration for patients with unmethylated MGMT | |||
status, and especially for those patients with unmethylated MGMT status and amplified | |||
EGFR. For patients unfit to receive the standard high dose temozolomide schedule, a very | |||
low dose metronomic schedule of TMZ may provide some benefit, perhaps through | |||
selective toxicity to immune suppressor cells, and in combination with COX-2 inhibition | |||
as in the German studies above. | |||
===How many cycles of TMZ?=== | |||
An important question is how long the use of TMZ should be continued. The Stupp | |||
clinical trial continued it for only six cycles after radiation, but many patients have | |||
continued that protocol for longer period of times. | |||
In what is perhaps the only randomized, prospective trial comparing different numbers of | |||
cycles of adjuvant temozolomide, 20 newly diagnosed glioblastoma patients were | |||
assigned to six cycles and another 20 patients were assigned to 12 cycles (355). Median | |||
progression-free survival outcomes were 12.8 months in the 6-month group and 16.8 | |||
months in the 12-month group, which was borderline statistically significant (p=0.069). | |||
Median overall survival was 15.4 versus 23.8 months, and achieved statistical significance | |||
despite the low numbers of patients included in the trial (p=0.044). A serious limitation | |||
of this study is that no information on MGMT status of the patients was collected, and | |||
therefore it’s possible that the proportion of patients with MGMT promoter methylated | |||
tumors was not equal in the two arms. | |||
A retrospective study done in Canada (51) compared patients who received the standard | |||
six cycles of temozolomide with those who had more than six cycles (up to 12) Patients | |||
receiving six cycles had a median survival of 16.5 months, while those receiving more than | |||
six cycles had a median survival of 24.6 months. | |||
The latest attempts to define the optimal length of monthly temozolomide (TMZ) therapy | |||
were published as abstracts for the SNO 2015 annual meeting. In the first of these studies | |||
(reference 325, abstract ATCT-08), a large team of investigators retrospectively analyzed | |||
data from four large randomized trials with the aim of comparing 6 cycles of monthly | |||
TMZ to >6 cycles. Only patients who had completed 6 cycles of TMZ and had not | |||
progressed within 28 days of completing cycle 6 were included. Important prognostic | |||
factors such as age, performance status, extent of resection and MGMT status were | |||
incorporated into the analysis. For these patients, treatment with more than 6 cycles of | |||
TMZ was associated with significantly improved progression-free survival [HR=0.77, | |||
p=0.03] independently of the examined prognostic factors, and was particularly beneficial | |||
for those with methylated MGMT status. Surprisingly, overall survival was not | |||
significantly different between the two groups (p=0.99). | |||
In the second abstract (reference 326, abstract ATPS-38), a Japanese group attempted to | |||
clarify whether more than 12 cycles of TMZ was beneficial in terms of increased survival. | |||
Patients in this study were divided into four groups: a) 12 cycles, b) 24 cycles, c) more | |||
than 24 cycles until relapse, and d) beyond 12 cycles (this group includes the b) and c) | |||
groups). 12, 14, 12, and 40 patients were included in each of these groups. No significant | |||
progression-free survival difference was detected between groups a) and b), implying a | |||
lack of benefit of 24 versus 12 cycles. Importantly, patients who were able to continue | |||
TMZ treatment for at least 12 cycles (all the patients in this study) had a median | |||
progression-free survival of 4.3 years and median overall survival of 6.3 years. This study | |||
failed to show a benefit of continuing TMZ cycles beyond 12. | |||
===Combining the Standard Treatment with Additional Agents=== | |||
Few oncologists believe that single-agent treatments are likely to be curative. The issue is | |||
finding the optimal combinations, based on toxicities and differences in the mechanisms | |||
of actions. Prior to the introduction of temozolomide, the PCV combination of | |||
procarbazine, CCNU, and vincristine had been the most widely used combination | |||
treatment for glioblastomas, but its use has never been shown to produce a better | |||
outcome than treatment with BCNU as a single agent. Nevertheless, there is now a large | |||
amount of research studying the effects of combining temozolomide with other therapies, | |||
most of which supports the view that such combinations improve treatment outcome, | |||
sometimes substantially. A variety of additional therapies are discussed in the following | |||
chapters. | |||
==Available Treatments== | |||
===Optune (formerly NovoTTF-100A) by Novocure=== | |||
{{#ask: [[Category:Innovative Cancer Therapies]] | |||
|?Has treatment name=Drug Name | |||
|?Has Usefulness Rating=Usefulness Rating | |||
|?Has OS with=OS_with | |||
|?Has OS without=OS_without | |||
|?Has Toxicity Level=toxicity_level | |||
|?Has Toxicity Explanation=toxicity_explanation | |||
|format=table | |||
}} | |||
{{#ask: [[Has treatment name::Optune (Optune Gio® for newer version)]] | |||
|?Has original text | |||
|format=template | |||
|template=CustomTextDisplay | |||
}} | |||
In the spring of 2011, the FDA approved the fourth treatment ever for glioblastoma. | |||
Unlike the previous three (gliadel, temozolomide, and Avastin), the new treatment | |||
involves no drugs or surgery, but instead uses a “helmet” of electrodes that generates a | |||
low level of alternating electrical current. A biotech company called Novocure has | |||
developed the device, called Optune, based on experimental findings that electro- | |||
magnetic fields disrupt tumor growth by interfering with the mitosis stage of cell | |||
division, causing the cancer cells to die instead of proliferating (138). Healthy brain cells | |||
rarely divide and thus are unaffected. The treatment involves wearing a collection of | |||
electrodes for 18 or more hours per day, which allows the patient to live otherwise | |||
normally. This approval in 2011 was the outcome of a randomized phase 3 trial for | |||
recurrent glioblastoma, in which Novo-TTF (now called Optune) treatment was equally | |||
effective as physician’s choice chemotherapy, but with reduced toxicity and better quality | |||
of life (139, 140). | |||
====Optune plus chemoradiation, the next standard of care?==== | |||
EF-14 is a phase 3 randomized clinical trial for newly diagnosed glioblastoma which | |||
compared standard of care chemoradiation followed by Optune (NovoTTF) and | |||
monthly cycles of Temodar, versus chemoradiation followed by monthly cycles of | |||
Temodar alone. | |||
In November 2014, at the annual SNO meeting in Miami Beach, Roger Stupp made a | |||
“late-breaking” presentation before a packed audience, describing interim survival | |||
outcomes from the EF-14 trial, essentially ushering in what may become the new standard | |||
of care for newly diagnosed glioblastoma. This trial is the first major phase 3 trial since | |||
the “Stupp protocol” was established in 2005 to report a positive, statistically significant | |||
survival benefit for newly diagnosed glioblastoma. In fact, the trial was so successful | |||
that it was terminated early and on December 2, Novocure announced that the FDA had | |||
approved an investigational device exemption (IDE) supplement allowing all the control | |||
patients in the EF-14 trial to begin receiving therapy with Optune tumor treating fields. | |||
�The interim results presented in Miami were based on the first 315 patients enrolled in | |||
the trial, who had at least 18 months of follow-up. Of these, 105 were randomized into the | |||
control arm and 210 were randomized to receive tumor treating fields. Survival and | |||
progression-free survival were measured from the time of randomization, which was a | |||
median of 3.8 months after diagnosis. Median progression-free survival was 7.1 months in | |||
the Optune arm versus 4 months in the control arm (hazard ratio 0.63, with a high degree | |||
of statistical significance, p=0.001). Median overall survival from randomization was 19.6 | |||
months in the Optune arm versus 16.6 months in the control arm (hazard ratio 0.75, | |||
statistically significant, p=0.034). 2-year survival was 43% in the Optune arm versus 29% | |||
in the control arm. It must be kept in mind that all these statistics are measured from | |||
randomization, roughly 4 months from diagnosis, meaning that median overall survival in | |||
the Optune arm approaches 24 months from diagnosis. The statistics above are for the | |||
intention-to-treat (ITT) population, which includes all patients randomized, as opposed | |||
to the as-treated (per-protocol) population, which excludes patients who did not start | |||
their second course of temozolomide or had major protocol violations. | |||
An October 5, 2015 press release announced that the FDA had approved Optune in | |||
combination with temozolomide for newly diagnosed glioblastoma, not quite a year after | |||
the first survival data from the trial was publicized. This is the first approval of a therapy | |||
for newly diagnosed glioblastoma since temozolomide was approved for this indication in | |||
March 2005. Two months later, in December 2015, the preliminary results of the EF-14 | |||
trial were published in the Journal of the American Medical Association (327). This | |||
publication detailed results for the first 315 patients enrolled, the same patients reported | |||
upon at the SNO 2015 annual meeting. Additional survival analysis on the per-protocol | |||
population (as opposed to the intention-to-treat population) gave an overall survival from | |||
randomization of 20.5 months in the Optune group and 15.6 months for the control group | |||
(that is, about 24.3 months and 19.3 months from diagnosis) (HR=0.64, p=0.004). | |||
Outcomes for the entire trial population of 695 patients were published for the 2016 SNO | |||
conference, with an updated press release from Novocure coming in April 2017. | |||
Confirming the results of the interim analysis, median progression-free survival was | |||
significantly improved in the Optune group by just under 3 months (6.7 versus 4 months | |||
from randomization). Median overall survival from randomization was improved by | |||
neatly five months (20.8 versus 16 months). Survival rate at 2 years from randomization | |||
was 42.5% in the Optune group versus 30% in the control group. The April 2017 update | |||
also reported on 5 year survival rate, which was 13% in the Optune arm versus 5% in the | |||
control arm. | |||
As of July 2016, the National Comprehensive Cancer Network (NCCN) had given Optune | |||
a 2A listing for newly diagnosed glioblastoma, indicating uniform consensus amongst the | |||
NCCN panel that this treatment is appropriate. As the NCCN is known as setting the | |||
standard treatment guidelines for cancer in the USA, this formalizes the concept of | |||
Optune as part of a new standard of care for newly diagnosed glioblastoma. Although its | |||
status as part of a new standard of care may still be disputed by some, Novocure has | |||
announced that Optune is now available at over 600 treatment centers in the USA (click | |||
here for a list of these US centers), as well as 350 additional institutions internationally, | |||
including locations in Germany, Switzerland, Austria, and Japan. | |||
=== Treatment Categories === | |||
Explore the various treatment categories for comprehensive insights and latest developments: | |||
{{#show: CBD | ?|treatment_category }} | |||
* [[:Category:Repurposed Drugs|Repurposed Drugs]] | |||
* [[:Category:Hormones|Hormones]] | |||
* [[:Category:Nutraceuticals|Nutraceuticals]] | |||
* [[:Category:Antibody-Drug Conjugates and other protein-drug conjugates|Antibody-Drug Conjugates and other protein-drug conjugates]] | |||
* [[:Category:Other Chemotherapy and Cancer Drugs|Other Chemotherapy and Cancer Drugs]] | |||
... | |||
=== Explore Treatments by Usefulness Rating === | |||
Discover treatments that have shown promising results. | |||
{{#ask: [[Has Usefulness Rating::4]] OR [[Has Usefulness Rating::5]] | |||
| ?Has treatment name | |||
|?Has Usefulness Rating=Usefulness Rating | |||
|?Has Toxicity Level=toxicity_level | |||
| format=table | |||
}} | |||
Visit our [[:Category:Highly Useful Treatments|Highly Useful Treatments]] page to explore treatments rated with a usefulness of 4 or 5. | |||
=== Hormones === | |||
Unlike traditional cancer chemotherapy, which kills cancer cells through directly cytotoxic | |||
mechanisms, a different approach may also prove to be effective: manipulation of the | |||
body’s balance of circulating hormones to achieve the most unwelcoming environment for | |||
the growth of tumors. | |||
{{#ask: [[Category:Hormones and Cancer Therapy]] | |||
|?Has treatment name=Name | |||
|?Has Usefulness Rating=Usefulness Rating | |||
|?Has Toxicity Level=toxicity_level | |||
|format=table | |||
}} | |||
=== Repurposed Drugs === | |||
There are a large number of drugs that were developed initially for various different | |||
purposes that subsequent laboratory research demonstrated to have significant | |||
anti-cancer properties. Given these old drugs have been used for years, have well-defined | |||
toxicity profiles, and are generally cheaper due to being off-patent, they offer the | |||
possibility of augmenting the benefits of the current standard treatment without | |||
significant additional toxicity. However, because their FDA approval is for different | |||
purposes, many if not most neuro-oncologists have been reluctant to take advantage of | |||
their possible benefits as components of a treatment cocktail. Some of these drugs have | |||
been investigated as single agents for brain cancer treatment and some have also been | |||
combined with the now standard Stupp protocol. | |||
{{#ask: [[Category:Repurposed Drugs]] | |||
|?Has treatment name=Drug Name | |||
|?Has Usefulness Rating=Usefulness Rating | |||
|?Has Toxicity Level=toxicity_level | |||
|format=table | |||
}} | |||
{{:Over-the-Counter Drugs and Supplements}} | |||
{{:Nutraceuticals and Herbals}} | |||
=== Other Chemotherapy and Cancer Drugs === | |||
Explore additional chemotherapy and cancer drug treatments: | |||
{{PropertyTableFormat|Other Chemotherapy and Cancer Drugs}} | |||
====CCNU (lomustine)==== | |||
A report from Germany combined TMZ with CCNU (lomustine), the nitrosourea | |||
component of the PCV combination (52). Patients (N=39) received CCNU on day 1 of | |||
each 6-week cycle, and TMZ on days 2-6. Eight patients received intensified doses of | |||
both drugs, with somewhat better survival results (but with substantially increased | |||
toxicity). For present purposes, the results of all patients are aggregated. Median survival | |||
time was 23 months, and survival rates were 47%, 26%, 18%, and 16% at 2, 3, 4, and5 | |||
years, respectively. Four of the 39 patients had no recurrence at the 5-year mark. Only 23 | |||
of the 39 patients were assessable for the status of the MGMT gene. Those with | |||
methylated MGMT had a median survival of 34 months, while those with unmethylated | |||
MGMT had a median survival of only 12.5 months. | |||
These results, including a 5-year survival rate of 16%, are among the best yet reported, | |||
albeit with a relatively small number of patients. But it also should be appreciated that | |||
patients who suffered a recurrence received extensive salvage therapy of various types, | |||
which may have contributed substantially to survival time. The addition of CCNU to | |||
standard therapy for newly diagnosed glioblastoma is currently being tested in a phase 3 | |||
trial in Germany. | |||
====BCNU (carmustine) and Gliadel (carmustine wafers)==== | |||
The combination of Temodar with BCNU, the traditional chemotherapy for glioblastomas, | |||
has also been studied, but has been complicated by issues of toxicity and the optimal | |||
schedule of dose administration for the two drugs. However, a recent published report | |||
involving patients with tumors recurring after radiation but no prior chemotherapy failed | |||
to show any benefit of combining BCNU with Temodar, compared to Temodar alone, as | |||
the PFS-6 for the combination was only 21%, accompanied by considerable toxicity (53). | |||
An important variation in the use of BCNU has been the development of polymer wafers | |||
known as gliadel. A number of such wafers are implanted throughout the tumor site at the | |||
time of surgery. BCNU then gradually diffuses from the wafers into the surrounding | |||
brain. A possible problem with the treatment is that the drug will diffuse only a small | |||
distance from the implant sites, and thus fail to contact significant portions of the tumor. | |||
However, a phase III clinical trial has demonstrated that survival time for recurrent high- | |||
grade gliomas is significantly increased by the gliadel wafers relative to control subjects | |||
receiving wafers without BCNU, although the increase in survival time, while | |||
statistically significant, was relatively modest (54). Probably the best estimate of the | |||
benefit of gliadel as an initial treatment comes from a randomized clinical trial, | |||
conducted in Europe (55), which reported a median survival of 13.9 months for patients | |||
receiving gliadel compared to a median survival of 11.6 months for patients implanted | |||
with placebo wafers. As with other forms of chemotherapy, larger differences were | |||
evident for long-term survival. After a follow-up period of 56 months, 9 of 120 patients | |||
who received gliadel were alive, compared to only 2 of 120 of those receiving the | |||
placebo. However, the results were not reported separately for glioblastomas vs. other | |||
high-grade gliomas, suggesting that the outcome results would have been more modest | |||
for the glioblastoma patients alone. | |||
When gliadel has been combined with the standard TMZ + radiation protocol, survival | |||
time seems to be significantly improved, as assessed in three different retrospective | |||
clinical studies. In the first, from the Moffitt Cancer Center in Florida (56), the | |||
combination produced a median overall survival of 17 months, and a 2-year survival rate | |||
of 39%. In a second clinical trial reported by Johns Hopkins, where gliadel was | |||
developed (57), 35 patients receiving the combination had a median survival time of 20.7 | |||
months and a 2-year survival of 36%. In a third trial conducted at Duke University (58), | |||
36 patients receiving gliadel in addition to the standard TMZ protocol had a median | |||
survival of 20.7 months and a 2-year survival of 47%. The Duke cohort also received | |||
rotational chemotherapy (which included TMZ) subsequent to radiation. It is important | |||
to keep in mind that patients eligible to receive gliadel must have operable tumors, which | |||
excludes patients who have received a biopsy only and have a generally poorer prognosis | |||
as a result. The effect of this selection bias is difficult to evaluate but it is likely to | |||
account for a significant fraction of the improvement in survival time when gliadel | |||
+TMZ is compared to TMZ alone. | |||
A major advantage of gliadel is that it avoids the systemic side effects of intravenous | |||
BCNU, which can be considerable, not only in terms of low blood counts but also in | |||
terms of a significant risk of major pulmonary problems. But gliadel produces its own | |||
side effects, including an elevated risk of intracranial infections and seizures. However, | |||
the lack of systemic toxicity makes gliadel a candidate for various drug combinations. | |||
Especially noteworthy is a recent phase II trial with 50 patients with recurrent tumors | |||
that combined gliadel with 06-BG, a drug that depletes the MGMT enzyme involved in | |||
repair of chemotherapy-induced damage, but also causes unacceptable bone marrow | |||
toxicity when chemotherapy is given systemically. Survival rates at six months, one year | |||
and two years were 82%, 47%, and 10%, respectively (59) which seems notably better than | |||
the earlier clinical trial with recurrent tumors using gliadel without the 06-BG, in which | |||
the corresponding survival rates were 56%, 20%, and 10%. Median survivals were also | |||
notably improved by the addition of 06-BG (50.3 weeks versus 28 weeks). | |||
====Platinum compounds==== | |||
An improvement in results relative to those obtained with Temodar alone has also been | |||
reported when Temodar has been combined with cisplatin. In a pair of clinical studies | |||
performed in Italy (61, 62) with patients with recurrent tumors, the PFS-6 was 34% and | |||
35%. A treatment protocol with newly diagnosed patients that also seems to have | |||
produced better results than Temodar as a single agent combined Temodar with both | |||
cisplatin and etoposide (VP-16), given through the carotid artery (63). Cisplatin and | |||
etoposide were given after surgery and continued for three cycles spaced every 3 weeks | |||
apart, followed by the standard protocol of radiation plus low-dose Temodar, then | |||
high-dose Temodar on the schedule of days 1-5 of every month. For 15 patients studied, | |||
median survival was 25 months. | |||
====Procarbazine==== | |||
Temodar has also been combined with procarbazine (64). While the report of that study | |||
did not include the PFS-6 statistic, it did report an unusually high percentage of tumor | |||
regressions, suggesting that this combination might be effective. | |||
====Bevacizumab (Avastin)==== | |||
The most notable development in drug combinations has been the addition of the anti- | |||
angiogenic drug, Avastin (also known as bevacizumab), to the standard Stupp protocol. | |||
As will be discussed later, Avastin has FDA approval for the treatment of glioblastomas | |||
that have recurred or progressed after initial treatment. Several clinical trials have now | |||
investigated its combination with the gold standard Temodar protocol. | |||
Recently, there have been two large randomized phase III clinical trials comparing | |||
the Stupp protocol and the Stupp protocol + Avastin, for newly diagnosed patients. In the | |||
first of these (70), known as the AVAglio trial, median PFS was 10.6 months for those | |||
receiving Avastin versus 6.2 months for those receiving only the Stupp protocol, a | |||
statistically significant difference. However, median overall survival was not different | |||
(16.8 months vs. 16.7 months). It should be noted that patients in the control group | |||
typically received Avastin after tumor progression occurred, so that the comparison was | |||
really between Avastin given early versus Avastin given only after recurrence. Additional | |||
results were that 72% of the Avastin group was alive at one year, compared to 66% of the | |||
control group, while two year survival was 34% vs. 30%. | |||
In the second of these large trials (71), conducted by the RTOG consortium, the design | |||
was essentially similar to the AVAglio trial, as were the results. Median PFS was 10 | |||
months for those receiving Avastin vs. 7.3 months for the control group (again statistically | |||
significant), while median overall survival was 15.7 months for the Avastin group | |||
compared to 16.1 months for the control, a nonsignificant difference. | |||
The best interpretation of these results is that patients have a longer time without tumor | |||
progression, and presumably a better quality of life, when Avastin is used as part of the | |||
initial treatment. However, there is no benefit for overall survival, when compared to | |||
withholding Avastin until recurrence is detected. An additional feature of the results, not | |||
emphasized by the authors of the reports, is that the overall survival times were not | |||
notably better, and in many cases worse, than those obtained when the Stupp protocol is | |||
combined with various other treatment agents. | |||
EGFR inhibitors: Iressa, Tarceva, and Erbitux (gefitinib, erlotinib, and | |||
cetuximab) | |||
These three drugs, which have FDA approval for several different types of cancer, have | |||
the common feature that they target a growth-signaling channel known as the epidermal | |||
growth factor. Overexpression or mutation of EGF receptors is involved in the growth | |||
many different kinds of cancer, including more than half of glioblastomas. In general, use | |||
of these drugs as single agents has produced disappointing results, although occasional | |||
long-term survivors have occurred. More promising results have occurred when EGFR | |||
inhibitors have been used in combination with the Stupp protocol. | |||
When Tarceva has been added to the standard Temodar protocol for newly diagnosed | |||
patients, median survival was 15.3 months (N=97) in one study (72) and 19.3 months | |||
(N=65) in a second study (73). The results of the second study were compared to two | |||
previous phase II trials involving a similar patient population, in which Temodar was | |||
combined with either thalidomide or accutane. Median survival for those trials was 14.1 | |||
months. | |||
The moderately positive results of the just described trial are in conflict with a very | |||
similar trial (N=27) conducted at the Cleveland Clinic (74). In that trial median survival | |||
was only 8.6 months, notably worse than the outcomes obtained when temodar has been | |||
used without tarceva. How the conflicting results can be reconciled is unclear. | |||
Erbitux (also known as cetuximab) is a monoclonal antibody, which differs from Iressa | |||
and Tarceva, which are small molecules, Because monoclonal antibodies are not believed | |||
to cross the blood-brain barrier, the natural expectation is that Erbitux would be | |||
ineffective against brain tumors. As a single agent, this seems to be true, as PFS-6 was | |||
only 10% for patients with recurrent high-grade gliomas (75). But when Erbitux was | |||
added during the radiation phase of the standard temozolomide protocol for 17 newly | |||
diagnosed patients (76), 87% of patients were alive at the end of one year and 37% were | |||
progression free. The median survival time had not been reached at the time of the report | |||
(an abstract at a meeting). It is possibly important to note that some investigators believe | |||
that radiation temporarily disrupts the blood-brain-barrier, which would allow a | |||
monoclonal antibody such as erbitux to reach the tumor. | |||
An important development for identifying patients likely to respond to Tarceva has come | |||
from a study (77) of glioma patients whose tumor pathologies were also assessed for their | |||
levels of a second protein called PKB/AKT. This is a signaling channel that results from | |||
inactivation of the PTEN gene, a tumor suppressor gene commonly mutated in | |||
glioblastomas. None of the tumors with high levels of PKB/AKT responded to treatment | |||
with Tarceva, whereas 8 of 18 tumors with low levels did respond to the treatment. A | |||
refinement of this approach tested for three different proteins: expression of PTEN, | |||
expression of EGFR, and of a mutation of the EGFR protein known as EGFR variant III | |||
(78). The level of EGFR was not related to clinical outcome, whereas the co-expression | |||
of EGFR variant III and PTEN strongly predicted clinical outcome. | |||
Because the inhibition of PKB/AKT should plausibly increase the effectiveness of EGFR | |||
inhibitors, a treatment strategy now being tested is the combination of EGFR inhibitors | |||
with rapamycin (trade name rapamune, generic name sirolimus), an existing drug used | |||
for organ transplants to suppress the immune system and prevent organ rejection, but | |||
which also inhibits mTOR complex 1, a tumor growth promoter downstream of AKT. A | |||
phase I trial (79) combined Iressa with rapamycin for 34 patients (25 GBM) with | |||
recurrent tumors; two patients had a partial tumor regression and 13 patients achieved | |||
stable disease. PFS-6 was 24%. A second clinical trial (80) with 28 heavily pretreated | |||
patients with low performance status (median Karnofsky score of 60) received either | |||
Iressa or Tarceva in combination with rapamycin, with the result that 19% of patients had | |||
tumor regression while 50% had stable disease, with a PFS-6 value of 25%. Yet a third | |||
clinical trial (81) that combined tarceva and sirolimus for recurrent GBM had much worse | |||
results, with PFS-6 value of only 3%. | |||
The foregoing results of the use of EGFR inhibitors for GBM treatment range from | |||
moderately positive to minimal efficacy. The reasons for this variability are not obvious, | |||
although treatment efficacy is likely dependent on numerous genetic markers. Thus, | |||
without a genetic analysis of individual tumors, it is hard to see a basis for recommending | |||
their use. | |||
�One recent paper (83) of potential major importance has noted that tumors may not | |||
respond to anti-EGFR drugs because of activation of the gene for a second growth factor | |||
known as the insulin-like growth factor receptor I (IGF1R). IGF1R has also been | |||
implicated as a source of resistance to tamoxifen and various other treatment agents. It is | |||
noteworthy, therefore, that two of the supplements to be discussed, silibinin and | |||
lycopene, are known to inhibit IGF-I. This suggests that silibinin and lycopene might | |||
substantially increase the effectiveness of any treatment that relies on EGFR inhibition. | |||
Metformin, a widely used diabetes drug, is also known to reduce the level of IGF-1, | |||
currently is under investigation as a treatment for several different kinds of cancer. | |||
An important issue is how the effectiveness of EGFR inhibitors are related to the findings | |||
discussed earlier that metronomic schedules of Temodar produce a large survival | |||
improvement for GBMs that have EGFR overexpression. All of the clinical trials | |||
discussed in this section used the standard Temodar schedule, so it is unclear whether a | |||
metronomic schedule might produce different outcomes. | |||
====Gleevec (imatinib)==== | |||
Gleevec (also known as imatinib), a small molecule which targets a specific gene involved | |||
in the growth of a form of leukemia, received a great deal of publicity because of its | |||
unprecedented effectiveness. As will be discussed later, this general strategy of | |||
identifying the growth signals for tumor growth and then targeting those signals, or their | |||
receptors, is one of the major new areas in cancer research. Such growth signaling | |||
channels often are involved in several different types of cancer. Although Gleevec was | |||
developed specifically for chronic myelogenous leukemia, it also has been shown to | |||
inhibit a more general type of growth signal, platelet-derived growth factor (PDGF), | |||
which is also involved in the growth of gliomas and other forms of cancer (e.g., small- | |||
cell lung cancer). Laboratory research has supported the importance of this similarity in | |||
that gleevec has been shown to strongly inhibit glioma growth, with the result that there | |||
now have been a number of studies reporting its use with high-grade gliomas. | |||
The generally disappointing results using gleevec for brain tumors may have occurred | |||
for several different reasons. It may not readily cross the blood-brain-barrier, and it may | |||
engender different mechanisms of resistance than other treatment agents. In the study of | |||
gleevec for leukemia, for example, high levels of autophagy have been observed, which | |||
can be inhibited by the concurrent use of chloroquine or other autophagy inhibitors. | |||
An important variation in the use of gleevec was to restrict its usage to patients with | |||
recurrent tumors who tested positive for overexpression of the platelet-derived growth | |||
factor receptor (90). PDGFR is overexpressed in 50-65% of tumors, especially tumors | |||
labeled secondary glioblastomas, which are believed to have evolved from lower-grade | |||
tumors (in contrast to de novo glioblastomas that occur without such evolution). For this | |||
restricted patient population, the PFS-6 value was 53%. | |||
=== Treatments for Recurrent Glioblastoma === | |||
While Temodar is now the drug of choice for the initial treatment of glioblastoma, the | |||
majority of patients will receive minimal benefit. Patients who have failed the standard | |||
treatment protocol often proceed to other chemotherapy drugs. These include the | |||
nitrosoureas, BCNU and CCNU (and ACNU in Europe and Japan), and also the platinum | |||
drugs, and irinotecan, a drug developed for colon cancer known also known as CPT-11. | |||
{{#ask: [[Category:Other chemotherapy agents at recurrence]] | |||
|?Has treatment name | |||
|?Has OS without=Overall Survival without PBT | |||
|?Has OS with=Overall Survival with PBT | |||
|?Has PFS without=Progression-Free Survival without PBT | |||
|?Has PFS with=Progression-Free Survival with PBT | |||
|?Has Usefulness Rating=Usefulness Rating | |||
|?Has Toxicity Level=toxicity_level | |||
|?Has Toxicity Explanation=Toxicity Explanation | |||
|format=table | |||
}} | |||
==Promising new Treatments == | |||
=== Antibody-Drug Conjugates and other protein-drug conjugates === | |||
Investigate the cutting-edge Antibody-Drug Conjugates and other protein-drug conjugates being developed: | |||
{{PropertyTableFormat|Antibody-Drug Conjugates and other protein-drug conjugates}} | |||
===Immunological Approaches=== | |||
Because cancer cells have a genetic structure different from normal cells they generate | |||
foreign proteins that in principle should be detected by the immune system and evoke the | |||
same type of immune reaction as any foreign virus or bacteria. This basic fact suggests | |||
that augmenting one's immune system might be an effective approach to cancer | |||
treatment. Such an approach has an immediate appeal because it is surely preferable to | |||
reinforce the immune system than to poison the entire body in the hope the cancer cells | |||
will be killed before the body is depleted of vital resources. However attractive this | |||
philosophy may be, translating it into an effective cancer treatment has proven to be | |||
extraordinarily difficult. Contrary to general belief, immunological treatments are not | |||
�benign to implement. Interferon treatment has very definite debilitating effects, as do | |||
cytokines such as interleukin-2 and tumor necrosis factor, because their modus operandi | |||
are essentially to create an inflammatory immune reaction not unlike a severe allergic | |||
reaction. When this inflammatory process is too severe, it can in fact be fatal. | |||
==== Vaccines ==== | |||
The holy grail of immunological approaches to cancer treatment is the development of | |||
effective vaccines. In principle this should be possible because of the differences in the | |||
protein structure of cancer cells and normal cells. But, two general problems must be | |||
overcome. The first is that different individuals have tumors with different collections of | |||
antigens (proteins), so that generic vaccines are unlikely to be effective; thus patient- | |||
specific vaccines are required. The second problem is that the immune system is not an | |||
efficient detector of the tumor's foreign antigens. In part this is due to the tumor secreting | |||
enzymes that in effect provide a protective cloak preventing such detection. The larger the | |||
tumor the stronger is its defense mechanisms to counteract immune-system detection. | |||
This is one reason that most vaccines work best when there is a minimum of tumor | |||
burden. | |||
=====Personalized vaccines===== | |||
======DCVax and other lysate-pulsed dendritic cell vaccines====== | |||
=====Tumor-associated antigen vaccines===== | |||
{{PropertyTableFormat|Tumor-associated antigen vaccines}} | |||
based on this book: [https://virtualtrials.org/pdf2017/treatment_options_gbm_2017.pdf Treatment Options for GBM - 2017 By Ben Williams] | |||
If you want to add treatments, you can use [https://chatgpt.com/g/g-N3d5rwrSJ-glioblastomatreatments-wiki-helper this GPT to help research and format the results] | |||
<comments /> | |||
Latest revision as of 11:04, 1 January 2025
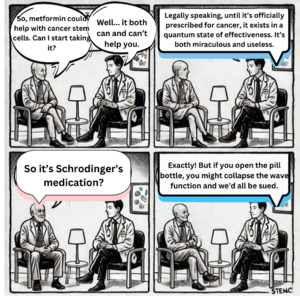
Since my own diagnosis of glioblastoma (GBM) in 1995 at age 50, I have spent considerable time researching treatment options, and the following discussion summarizes what I have learned. Most of the information is from medical journals and the proceedings of major cancer conferences. Some information has been contributed by others to various online brain tumor patient support groups, which I have followed up on, and some is from direct communications with various physicians conducting the treatments that are described. References are presented at the end for those who would like their physicians to take this information seriously. Although this discussion is intended to be primarily descriptive of the recent development of new treatment options, it is motivated by my belief that single-agent treatment protocols are unlikely to be successful, and patients are best served if they utilize multiple treatment modalities, and go beyond the “certified” treatments that too often are the only treatment options offered.
A more extensive account of my philosophy of treatment, and the reasons for it, are provided in my (2002) book, Surviving "Terminal" Cancer: Clinical Trials, Drug Cocktails, and Other Treatments Your Doctor Won't Tell You About. Currently, it is available only at Amazon.com, where reviews of the book also are available.
When I began my search for effective treatments, the available options offered little chance for surviving my diagnosis. The standard treatment included surgery, radiation, and nitrosourea-based chemotherapy, either BCNU alone or CCNU combined with procarbazine and vincristine (known as the PCV combination). While this treatment has helped a small minority of people, its 5-year survival rate has been only 2-5%. Median survival has been about a year, which is 2-3 months longer than for patients receiving radiation alone without chemotherapy. Fortunately, as will be discussed in the next section, the past ten years has produced a new “gold standard” of treatment for newly diagnosed patients: the combination of radiation with a new chemotherapy agent, temozolomide (trade name Temodar in the USA and Temodal elsewhere in the world). While this new standard appears to produce a notable improvement over previous treatments, it still falls far short of being effective for the great majority of patients.
Also available now are three other treatments that have FDA approval for tumors that have recurred or have progressed after initial treatment: Gliadel, Avastin, and an electrical field therapy named Optune (formerly known as NovoTTF). All of these are considered standard of care for recurrent tumors (which is important for insurance reasons), and can legally also be used for newly diagnosed patients as well. Each will be discussed later in this article. There are three general premises to the approach to treatment that will be described. The first is borrowed from the treatment approach that has evolved in the treatment of AIDS. Both viruses and cancer cells have unstable genetic structures susceptible to mutations. This implies that the dynamics of evolution will create new forms that are resistant to whatever the treatment may be. However, if several different treatments are used simultaneously (instead of sequentially, which is typically the case), any given mutation has a smaller chance of being successful. A mathematical model instantiating these assumptions has recently been developed and has been shown to describe the pattern of tumor growth for melanoma (1).
The second premise is that cancer treatments of all sorts are probabilistic in their effects. None work for everyone, in part because any given cancer diagnosis is an amalgam of different genetic defects that respond in different ways to any given treatment agent. This is especially true for glioblastomas, which have a multiplicity of genetic aberrations that vary widely across individuals and sometimes even within the same tumor of a given individual. As a result it is common that any given "effective" treatment agent will
benefit only a minority of patients, often in the range of 10-35%, but do little if anything for the majority. The result is that the chances of finding an effective treatment increase the more different treatment agents that are utilized. Probabilistic effects can and do summate.
An important implication of the genetic diversity of GBM tumors is that tests of treatment agents presented individually will often fail, not because they lack effectiveness, but because they target only one or sometimes two growth pathways, leaving other growth pathways to be upregulated to maintain the growth of the tumor. Thus, even at the level of clinical trials, tests of individual treatment agents in isolation may be a misguided strategy. A drug that fails in isolation might in fact be effective when combined with other drugs that target the additional alternative growth pathways.
A third general principle is that any successful treatment needs to be systemic in nature because it is impossible to identify all of the extensions of the tumor into normal tissue. Moreover, cancer cells are typically evident in locations in the brain distant from the main tumor, indicating that metastases within the brain can occur, although the great majority of tumor recurrences are within or proximal to the original tumor site. Localized treatments such as radiosurgery may be beneficial in terms of buying time, but they are unlikely to provide a cure, except in cases when the tumor is detected early and is very small. Even if the localized treatment eradicates 99% of the tumor, the small amount of residual tumor will expand geometrically, eventually causing significant clinical problems.
Until the development of immunological treatments in just the last few years, which will be discussed in a later section, the only systemic treatment available has been cytotoxic chemotherapy, which historically has been ineffective except for a small percentage of patients. An important issue, therefore, is whether chemotherapy can be made to work substantially better than it typically does. Agents that facilitate or augment its effects are critically important. As will be seen, a number of older drugs developed for other purposes have been shown in laboratory studies to be effective against cancer, often with minimal toxicity. The availability of these treatments raises the possibility that some combination of these new agents can be packaged that provide effective treatment based on several different independent principles. Thus, the AIDS-type of combination approach is now a genuine possibility whereas it would not have been fifteen years ago. Because many of these relatively nontoxic new agents were developed for purposes other than cancer, or for different kinds of cancer, their utilization in the treatment of glioblastomas is "off-label", with the result that many oncologists have been hesitant to prescribe them. Thus, patients themselves need to become familiar with these new agents and the evidence available regarding their clinical effectiveness. It is possible, although by no means proven, that some combination of these newly repurposed agents offers the best possibility for survival.
Patients may or may not learn about the treatments that will be described from their physicians. To appreciate why, it is important to understand how American medicine has been institutionalized. For most medical problems there is an accepted standard of what is the best available treatment. Ideally, such treatments are based on phase III clinical trials in which patients are randomly assigned to receive the new treatment or some type of control condition. Treatments that have been studied only in nonrandomized phase II trials will rarely be offered as a treatment option, even if the accepted "best available treatment" is generally ineffective. What happens instead is that patients are encouraged to participate in clinical trials. The problem with this approach is that most medical centers offer few options for an individual patient. Thus, even though a given trial for a new treatment may seem very promising, patients can participate only if that trial is offered by their medical facility. Yet more problematic is that clinical trials with new treatment agents almost always initially study that agent in isolation, usually with patients with recurrent tumors who have the worst prognoses. For newly diagnosed patients this is at best a last resort. What is needed instead is access to the most promising new treatments, in the optimum combinations, at the time of initial diagnosis.
In the discussion to follow, it is important to distinguish between treatment options at the time of initial diagnosis versus those when the tumor either did not respond to the initial treatment or responded for a period of time and then recurred. Different measures of treatment efficacy are often used for the two situations, which sometimes makes treatment information obtained in one setting difficult to apply to the other. The recurrent tumor situation is also complicated by the fact that resistance to the initial treatment may or may not generalize to new treatments given at recurrence. The Importance of Brain Tumor Centers
When someone is diagnosed with a brain tumor they are faced with a situation about which they know very little, but nevertheless must develop a treatment plan very quickly, because GBMs grow very rapidly if left untreated. The first step, if possible, is to have as much of the tumor removed as possible, because various data show substantially increased survival times for those with complete resections, relative to those who have incomplete resections or only biopsies. Accordingly, it is best that patients seek treatment at a major brain tumor center because neurosurgeons there will have performed many more tumor removals than general neurosurgeons that typically work in the community setting. This is especially important in recent times, as surgical techniques have become increasingly more sophisticated and utilize procedures that community treatment centers do not have the resources to perform. I know of numerous cases in which a local neurosurgeon has told the patient the tumor is inoperable, only to have the same tumor completely removed at a major brain tumor center.
An additional advantage of utilizing a major brain tumor center is that they are better equipped to do genetic analyses of tumor tissue, which are increasingly important in guiding treatment decisions. Moreover, they provide a gateway into clinical trials.
The Importance of Brain Tumor Centers
When someone is diagnosed with a brain tumor they are faced with a situation about which they know very little, but nevertheless must develop a treatment plan very quickly, because GBMs grow very rapidly if left untreated. The first step, if possible, is to have as much of the tumor removed as possible, because various data show substantially increased survival times for those with complete resections, relative to those who have incomplete resections or only biopsies. Accordingly, it is best that patients seek treatment at a major brain tumor center because neurosurgeons there will have performed many more tumor removals than general neurosurgeons that typically work in the community setting. This is especially important in recent times, as surgical techniques have become increasingly more sophisticated and utilize procedures that community treatment centers do not have the resources to perform. I know of numerous cases in which a local neurosurgeon has told the patient the tumor is inoperable, only to have the same tumor completely removed at a major brain tumor center.
An additional advantage of utilizing a major brain tumor center is that they are better equipped to do genetic analyses of tumor tissue, which are increasingly important in guiding treatment decisions. Moreover, they provide a gateway into clinical trials.
The Standard of Care for Initial Treatment
Glioblastoma
Although chemotherapy has a long history of being ineffective as a treatment for glioblastoma, a large randomized European-Canadian clinical trial (EORTC trial 26981/22981) has shown clear benefits of adding the new chemotherapy agent, temozolomide (trade name Temodar in the USA, Temodal elsewhere in the world) to the standard radiation treatment (2). This treatment, followed by 6 or more monthly cycles of temozolomide, has become known as the “Stupp protocol” after Roger Stupp, the Swiss oncologist who led the trial. In this trial, one group of patients received radiation alone; the other group received radiation plus Temodar, first at low daily dosages during the six weeks of radiation, followed by the standard schedule of higher-dose Temodar for days 1-5 out of every 28-day cycle. Median survival was 14.6 months, compared to a median survival of 12 months for patients receiving radiation only, a difference that was statistically significant. More impressive was the difference in two-year survival rate, which was 27% for the patients receiving temodar but 10% for those receiving only radiation. Longer-term follow-up has indicated that the benefit of temozolomide (TMZ) persists at least up to five years: The difference in survival rates between the two treatment conditions was 16.4% vs. 4.4% after three years, 12.1% vs. 3.0% after four years, and 9.8% vs. 1.9% after five years (3). As a result of these findings, the protocol of TMZ presented during radiation is now recognized as the "gold standard" of treatment. Note, however, that all of these numbers are somewhat inflated because patients over the age of 70 were excluded from the trial.
In July of 2016, the National Comprehensive Cancer Network (NCCN) recommended Optune as a category 1 treatment for newly diagnosed glioblastoma in combination with the standard temozolomide-based chemotherapy (see press release here). This rating indicates a uniform consensus by the NCCN that this treatment is appropriate. As the NCCN is recognized as setting the standards for cancer treatment in the USA and in other countries abroad which follow its guidelines, Optune in combination with standard chemotherapy following radiation could now be considered to be a new standard of care for newly diagnosed glioblastoma. See more detailed information on Optune in Chapter 3.
Research summarized here: https://virtualtrials.org/optune/NVCR_Clinical_Evidence_Flipbook_9.5.23.pdf
Cancer Stem Cells (CSCs) in Glioblastoma: Challenges with Standard of Care (SOC)
What Are Cancer Stem Cells?
Cancer stem cells (CSCs) are a small subpopulation of cells within tumors that possess capabilities similar to those of normal stem cells, such as self-renewal and differentiation. In the context of glioblastoma, these cells are often referred to as glioma stem cells (GSCs). They are believed to be crucial drivers of tumor growth, resistance to treatment, and recurrence.
Standard of Care for Glioblastoma
The current standard of care for glioblastoma typically includes surgical resection followed by radiation therapy and chemotherapy with temozolomide. While these treatments can initially reduce tumor size and manage symptoms, they do not effectively target GSCs, which can survive treatments and cause tumor recurrence.
Why Does SOC Fail to Prevent Recurrence?
- Resistance to Treatment: GSCs are highly resistant to chemotherapy and radiation. They have efficient DNA repair mechanisms and can remain dormant during treatment, evading the effects of SOC that target rapidly dividing cells.
- Microenvironment Protection: GSCs reside in protective niches within the tumor microenvironment that shield them from the effects of SOC. These niches provide support and maintain the stem-like qualities of GSCs, promoting their ability to regenerate the tumor.
- Tumor Regeneration: After treatment, surviving GSCs can regenerate the tumor, often leading to a recurrence that is more aggressive and resistant to further treatment. This cycle is a significant challenge in the management of glioblastoma.
Research and Future Directions
Understanding the biology of GSCs has led to the exploration of targeted therapies aimed at these cells. Strategies include developing drugs that specifically target the molecular pathways essential for GSC survival and proliferation, disrupting the tumor microenvironment, and using immunotherapy to enhance the body's natural defenses against these cells.
Conclusion
The recurrence of glioblastoma post-SOC is largely due to the presence and behavior of GSCs. Efforts to improve glioblastoma treatment outcomes must focus on effectively targeting these cells. Ongoing research into the molecular and environmental underpinnings of GSCs holds promise for developing more effective therapies that can prevent recurrence and extend patient survival.
Note: While alternatives to SOC are not proven to always work, exploring such options is crucial because without trying different approaches, recurrence is almost guaranteed.
Alternative Therapies Targeting GSCs
Various alternative therapies have been explored for their potential to target glioma stem cells (GSCs) in glioblastoma. These are considered experimental and have been primarily studied in preclinical trials or ongoing research settings:
- Curcumin: This compound, derived from turmeric, has anti-inflammatory properties and has been studied for its potential to disrupt pathways involved in cancer stem cell growth and survival.
- Resveratrol: Found in grapes and berries, resveratrol has been researched for its ability to inhibit the growth of cancer stem cells and induce apoptosis in various cancer cell models, including glioblastoma.
- Sulforaphane: A compound in cruciferous vegetables like broccoli, sulforaphane targets cellular processes that are critical for cancer cell growth and survival, impacting cancer stem cells.
- CBD: Research suggests that CBD may affect glioblastoma by targeting the stem-like properties of GSCs, potentially reducing their ability to contribute to tumor growth.
- Metformin: While primarily used for diabetes management, metformin has shown potential in preclinical studies for its anti-cancer effects and ability to target cancer stem cells in glioblastoma.
- Disulfiram: Traditionally used for treating alcohol dependency, disulfiram has been studied for its capacity to target cancer stem cells in glioblastoma, particularly when used in combination with copper.
- Parthenolide: This compound, from the herb feverfew, is being researched for its ability to induce oxidative stress and apoptosis in glioblastoma stem cells.
- Repurposed Drugs: Drugs approved for other conditions, such as antidepressants or antipsychotics, have been explored for their ability to interfere with signaling pathways critical for the maintenance of cancer stem cells and tumor resistance.
These therapies are still under investigation for their effectiveness and safety in treating glioblastoma and are generally considered for clinical trial settings. Patients should consult with healthcare professionals and consider clinical trials where these treatments are being tested.
Anaplastic astrocytoma
Though the “Stupp protocol” of combined temoradiation (concomitant radiation and temozolomide chemotherapy) followed by monthly cycles of temozolomide has been routinely applied to anaplastic astrocytoma patients, prospective confirmation of this use in this patient population has awaited results of the “CATNON” randomized phase 3 trial for 1p/19q non-codeleted grade 3 gliomas. Results of the interim analysis for this trial were first released for the ASCO 2016 annual meeting. Between 2007 and 2015, 748 patients were randomized to receive either i) radiation alone, ii) radiation with concomitant temozolomide, iii) radiation followed by 12 adjuvant monthly cycles of temozolomide, or iv) radiation with temozolomide both concurrently and with follow-up monthly cycles. At the time of the interim analysis (October 2015), significant progression-free and overall survival benefit was found with adjuvant temozolomide treatment (arms iii and iv). Median progression-free survival was 19 months in arms i and ii (not receiving adjuvant temozolomide) versus 42.8 months (receiving adjuvant temozolomide). 5-year survival rate was 44.1% and 55.9% in arms i and ii versus iii and iv. Median survival was not yet reached for arms iii and iv.
This analysis did not address the benefit of temozolomide concurrent with radiation, a question that will be answered with further follow-up, and studies assessing the impact of IDH1 mutation and MGMT methylation were still ongoing.
Determining who will benefit
A two-year survival rate of less than 30% obviously cannot be considered an effective treatment, as the great majority of patients receiving the treatment obtain at best a minor benefit, accompanied with significant side effects (although Temodar is much better tolerated than previous chemotherapy treatments, especially with respect to the cumulative toxicity to the bone marrow). This raises the issues of how to determine who will benefit from the treatment, and, most importantly, how to improve the treatment outcomes.
One approach to determining whether an individual patient will benefit from chemotherapy is simply to try 1-2 rounds to see if there is any tumor regression. The debilitating effects of chemotherapy typically occur in later rounds, at which point there is a cumulative decline in blood counts. The extreme nausea and vomiting associated with chemotherapy in the mind of the lay public is now almost completely preventable by anti-nausea agents, including Zofran (ondansetron), Kytril (granisetron) and Emend. (aprepitant). Marijuana also can be very effective in controlling such effects, and recent research has suggested that it has anti-cancer properties in its own right. Thus, for those patients who are relatively robust after surgery and radiation, some amount of chemotherapy experimentation should be possible without major difficulties.
An alternative way to ascertain the value of chemotherapy for an individual patient is the use of chemosensitivity testing for the various drugs that are possible treatments. Such testing typically requires a live sample of the tumor and thus must be planned in advance of surgery. Culturing the live cells is often problematic, but a number of private companies across the country offer this service. Costs range from $1000-$2500, depending on the scope of drugs that are tested. Such testing is controversial, in part because the cell population evolves during the process of culturing, which results in cells possibly different in important ways from the original tumor sample. Nevertheless, recent evidence has shown that chemosensitivity testing can enhance treatment effectiveness for a variety of different types of cancer, including a recent Japanese study using chemosensitivity testing with glioblastoma patients (4). However, this study did not involve cell culturing but direct tests of chemosensitivity for cells harvested at the time of surgery. In general, when chemosensitivity testing indicates an agent has no effect on a patient's tumor the drug is unlikely to have any clinical benefit. On the other hand, tests indicating that a tumor culture is sensitive to a particular agent do not guarantee clinical effectiveness, but increase the likelihood that the agent will be beneficial.
The Role of MGMT
A significant advance in determining which patients will benefit from Temodar was reported by the same research group that reported the definitive trial combining Temodar with radiation. Tumor specimens from the patients in that trial were tested for the level of activation of a specific gene involved in resistance to alkylating chemotherapy (which includes temozolomide and the nitrosoureas, BCNU, CCNU, and ACNU). full text
Dexamethasone
Most glioma patients will be exposed to dexamethasone (Decadron) at some point, as this corticosteroid is the first-line treatment to control cerebral edema caused by the leaky tumor blood vessels. Many also require dexamethasone during radiotherapy, and perhaps beyond this time if substantial tumor remains post-resection. Dexamethasone is an analog to the body’s own cortisol, but is about 25 times more potent. Though often necessary, dexamethasone comes with a long list of adverse potential side effects with prolonged use, including muscle weakness, bone loss, steroid-induced diabetes, immunosuppression, weight gain, and psychological effects.
New evidence also shows an association between dexamethasone use and reduced survival time in glioblastoma. This evidence has to be weighed against the fact that uncontrolled cerebral edema can be fatal in itself, and that dexamethasone is often required for its control. However, the attempt should always be made to use dexamethasone at the lowest effective dose, and to taper its use after control of edema is achieved, under a physician’s guidance.
In a retrospective study of 622 glioblastoma patients treated at Memorial Sloan Kettering Cancer Center, multivariate regression analysis showed an independent negative association of steroid use at the start of radiotherapy with survival (324). A similar negative association with survival outcomes was found in patients in the pivotal phase 3 trial that led to temozolomide being approved for glioblastoma in 2005, and for a cohort of 832 glioblastoma patients enrolled in the German Glioma Network.
Follow up studies in mice helped elucidate these retrospective clinical observations. In a genetically engineered PDGFB-driven glioblastoma mouse model, dexamethasone alone had no effect on survival, but pretreatment with dexamethasone for 3 days prior to a single dose of 10 Gy radiation negatively impacted the efficacy of radiation. This negative impact of dexamethasone on radiation efficacy was even more dramatic with multiple doses of dexamethasone given before 5 treatments with 2 Gy radiation, which more closely mimics what GBM patients are exposed to. In contrast, an antibody against VEGF, which could be considered a murine surrogate for Avastin, did not interfere with the efficacy of radiation.
In vivo mechanistic examination revealed that dexamethasone may interfere with radiation by slowing proliferation, leading to a higher number of cells in the more radioresistant G1 phase of the cell cycle, and fewer cells in the more radiosensitive G2/M phase. This finding has far-reaching implications about the potential interference by drugs with cytostatic mechanisms of action on the efficacy of radiation therapy.
The authors conclude by suggesting that antibodies against VEGF, most notably bevacizumab (Avastin), could be used as an alternative anti-edema drug during radiation in place of steroids. However, this use has to be weighed in importance against the exclusion from certain promising clinical trials due to prior use of Avastin being an exclusion criteria in some of these trials.
Radiation
The Role of Radiation
For many years the only treatment (other than surgery) offered to patients with glioblastomas was radiation, due to radiation being the only treatment found to improve survival time in randomized clinical trials. This continued to be the case in Europe until the last decade, but in this country chemotherapy (usually BCNU) gradually came to be accepted as a useful additional treatment component despite the absence of definitive evidence from clinical trials. Part of the reason for this acceptance of chemotherapy has been that very few patients receiving only radiation survive longer than two years (3- 10%), compared to 15-25% of patients also receiving chemotherapy.
The initial approach to using radiation to treat gliomas was whole-head radiation, but this was abandoned because of the substantial neurological deficits that resulted, sometimes appearing a considerable time after treatment. Current clinical practice uses a more focused radiation field that includes only 2-3 cm beyond the periphery of the tumor site. Because of the potential for radiation necrosis, the current level of radiation that is considered safe is limited to 55-60 Gy. Even at this level, significant deficits may occur, often appearing several years after treatment. The most common causes of these deficits are damage to the myelin of the large white fibers, which are the main transmitters of information between different centers of the brain, and damage to the small blood vessels, which results in an inadequate blood supply to the brain and also increases the likelihood of strokes. An additional risk, not yet proven clinically because of the typical short survival times of glioblastoma patients, is the growth of secondary tumors due to the radiation damage to the DNA. However, experimental work with animal models has supported the reality of this risk (208). Three-year-old normal rhesus monkeys were �given whole brain radiation using a protocol similar to the common human radiation protocol and then followed for 2-9 years thereafter. A startling 82% of the monkeys developed glioblastoma tumors during that follow-up period. It is currently unclear to what degree a similar risk occurs for human patients who are long-term survivors.
The major additional use of radiation in the treatment of gliomas has been localized radiation to the tumor field, after the external-beam radiation treatment is finished (or sometimes concurrently), either by use of implanted radiation seeds (typically radioactive iodine), a procedure known as brachytherapy, the use of radiosurgery (including gamma knife), or by the insertion into the tumor cavity of an inflatable balloon containing radioactive fluid (gliasite). Previous editions of this treatment summary devoted considerable discussion to these treatments. However, these treatments now are used much less frequently. Two different randomized trials of brachytherapy failed to show a statistically significant survival benefit even though the procedure causes considerable toxicity in terms of radiation necrosis (209). A recent randomized study of radiosurgery (210) similarly failed to show a benefit. Gliasite has yet to be studied in a randomized trial.
The usual interpretation of the failure to find a benefit in the randomized trials is that the initial studies indicating a survival benefit (usually increasing survival time about a year) involved a highly selected patient population, who otherwise had a good prognosis regardless of whether they received the procedure. However, selection bias seems not to account for all of the benefits of the procedure. For example, the use of gliasite for recurrent GBM tumors produced a median survival time of 36 weeks (211), which compares favorably with a median survival time of only 28 weeks when gliadel wafers were implanted for recurrent tumors, even though eligibility criteria were similar for the two procedures. Moreover, when patients receiving gliasite as part of the initial treatment (212) were partitioned according to according to established prognostic variables, and each partition was compared to its appropriate historical control, survival time was greater for patients receiving gliasite in each of the separate partitions.
Perhaps the best results reported involving radiation boosts comes from the combination of permanent radioactive iodine seeds with gliadel (212). Median survival for patients with recurrent glioblastomas was 69 weeks, although accompanied by considerable brain necrosis. The use of gliadel alone in the same treatment center, by comparison, produced a median survival time of 28 weeks, while the use of the radiation seeds alone produced a median survival of 47 weeks.
Impressive results have also been obtained with the addition of fractionated radiosurgery to the standard Stupp protocol for newly diagnosed patients (213). For 36 GBM patients median survival (from diagnosis) was 28 months and two-year survival was 57%. Median progression-free survival (from study entry) for the GBM patients was 10 months. �The foregoing results suggest that supplementary radiation procedures do provide some benefit, but it is important to appreciate that all only a portion of patients will be eligible for such treatment. Radiation necrosis caused by the treatment must be considered as well.
Hyberbaric oxygen and other radiosensitizers
A potentially important modification of the standard radiation protocols involves the use of hyperbaric oxygen prior to each radiation session. In a study conducted in Japan (214), 57 high-grade glioma patients received the standard radiation protocol with the addition of hyperbaric oxygen 15 minutes prior to each radiation session. Four rounds of chemotherapy were also administered, the first during the radiation period of treatment. For the 39 glioblastoma patients, the median survival time was 17 months, with a very high rate of tumor regression. For the 18 patients with anaplastic astrocytoma, median survival was 113 months. Two-year survival was reported separately for recursive partioning categories I-IV and V-VI, the latter including only glioblastoma patients. For categories I- IV, two-year survival was 50%; for categories V and VI, two-year survival was 38%. A long-standing goal of radiation oncology has been to find a radiation sensitizer that does not increase toxicity to normal tissue. One of the most promising advances toward this goal was reported at the 2011 ASCO meeting (215). A new drug derived from the taxane family, with the name OPAXIO, was combined with the standard Temodar + radiation protocol during the radiation phase of the treatment. The response rate for 25 patients (17 GBM) was 45% with 27% having a complete response. With a median follow-up of 22 months, median progression-free survival was 14.9 month (13.5 months for GBM patients). Median overall survival had not been reached at the time of the report. Note that the median PFS for the standard treatment without OPAXIO is 6.9 months.
Proton radiation therapy
| Common Side Effects | Overall Survival without PBT | Overall Survival with PBT | Progression-Free Survival without PBT | Progression-Free Survival with PBT | Usefulness Rating | toxicity_level | Toxicity Explanation | |
|---|---|---|---|---|---|---|---|---|
| Proton Radiation Therapy | Radiation dermatitis, temporary alopecia, radiation otitis, radiation necrosis (more prevalent in PBT group) | Data varies; traditional radiation therapies offer median OS of around 16-21 months for glioblastoma | High-dose PBT showed a median OS of 65.6 months for patients with radiation necrosis, and 26.9 months for patients without radiation necrosis in specific studies | Standard radiation therapy PFS rates are lower compared to PBT | Improved PFS observed with PBT, specific rates vary by study | 4 | 3 | While acute radiation-related toxicities were equivalent to conventional radiation therapy, PBT has a higher prevalence of radiation necrosis, indicating a need for careful patient selection and management. |
An alternative to the standard X-ray radiation is the use of proton beams, although only a few treatment centers have the required equipment. To date, there has been no meaningful comparison of the efficacy of proton-beam radiation and the normal procedure. However, one recent study in Japan did report unusually positive results when the two forms of radiation were combined, the standard procedure in the morning, and the proton-beam radiation in the afternoon (216). Also used was ACNU, a chemical cousin of BCNU and CCNU. Median survival for 20 patients was 21.6 month, with -1- year and 2-year progression-free rates of 45% and 16%. However, there were six cases of radiation necrosis that required surgery, indicating a considerably higher toxicity than normally occurs with the standard radiation procedure.
Gamma Knife Radiosurgery (GKRS) for GBM
| Common Side Effects | Overall Survival without GKRS | Overall Survival with GKRS | Progression-Free Survival without GKRS | Progression-Free Survival with GKRS | Usefulness Rating | toxicity_level | Toxicity Explanation | |
|---|---|---|---|---|---|---|---|---|
| Gamma Knife Radiosurgery | Lower compared to traditional GBM treatments, with no significant radiation-induced toxicities reported in recent studies. | 14-16 months with standard treatment. | Comparable to standard treatment, specifics depend on individual patient factors. | Typically, tumors recur within 6 months of standard treatment. | 5.6 months reported in recent studies using fractionated sessions with Gamma Knife ICON. | 3 | 2 | GKRS, especially when utilized in a fractionated approach with the Gamma Knife ICON, presents a viable treatment option for GBM patients, emphasizing reduced side effects while maintaining efficacy. |
The Gamma Knife radiosurgery (GKRS) for glioblastoma (GBM) showcases a potential treatment path with a lower toxicity profile, according to recent studies. This method, particularly through fractionated sessions using the Gamma Knife ICON, maintains progression-free and overall survival rates comparable to conventional treatments. The advantage lies in its safety and practicality for specific GBM patients, highlighting an approach that balances efficacy with reduced side effects. For detailed insights, refer to the study in BMC Cancer [here](https://bmccancer.biomedcentral.com/articles/10.1186/s12885-022-10162-w).
Radiation via Monoclonal Antibodies
An alternative for providing a radiation boost beyond the standard external field radiation involves attaching radioactive iodine-131 to a monoclonal antibody that targets a specific antigen, tenascin, which occurs on almost all high-grade glioma tumors and not on normal brain cells. The monoclonal antibodies are infused directly into the tumor cavity over a period of several days, and reportedly produces much less radiation necrosis than either brachytherapy or radiosurgery. The median survival time from a phase 2 clinical trial of this treatment for recurrent GBM tumors was 56 weeks (217). In the first study that reported using this approach as initial treatment (218) patients received the monoclonal antibodies, followed by the standard external-beam radiation and then a year of chemotherapy. Of 33 patients, only one required re-operation for necrotic tissue caused by the radiation. Median survival time was 79 weeks for the patients with glioblastoma (27 of 33 of total patients) and 87 weeks for all patients. Estimated two-year survival rate for GBM patients was 35%. A subsequent report of the results for an expanded number of patients indicated a mean progression-free survival of 17.2 months, compared to 4-10 months for other treatment procedures (219). Median overall survival measured from the time of diagnosis was 24.9 months. At the present time, however, only one treatment center (Duke University) has used this procedure. A multi-center clinical trial was planned, but the company sponsoring the trial apparently has shelved those plans for the indefinite future. A second type of monoclonal antibody treatment, developed at Hahneman University Medical School in Philadelphia, targets the epidermal growth factor receptor, which is overexpressed in the majority of GBM tumors (220) For patients who received the MAB treatment in combination with standard radiation, median survival time was 14.5 months; For patients who received the same protocol but with the addition of temodar, median survival was 20.4 months. A third type of monoclonal antibody, named Cotara, is designed to bind with proteins that are exposed only when cells are dying, with the result that adjacent living tumor cells are radiated by the radiation load carried by the monoclonal antibody. This rationale is based on the fact that that centers of GBM tumors have a large amount of necrosis. This approach has been under development by Peregrine Pharmaceuticals, a small biotech with limited funding. Recently they reported the long-term results from 28 recurrent GBM patients studied over a nine-year period (221). Seven of the 28 patients survived more than one year, while 3 of the 28 survived longer than five years (2 more than 9 years). Median survival was 38 weeks.
Strategies for improving the Standard of Care
Combatting chemoresistance
There are several ways that cancer cells evade being killed by cytotoxic chemotherapy. Already mentioned is that the damage inflicted by the chemotherapy is quickly repaired before actually killing the cell (due to the activity of the MGMT repair enzyme). A second source of resistance is that the chemo agent is extruded from the cancer before the next cell division (chemotherapy typically affects only those cells in the process of dividing). A third way is that the chemo agent doesn’t penetrate the blood-brain barrier. While Temodar is generally believed to cross the blood-brain-barrier effectively, empirical studies of its concentration within the tumor tissue have shown that its penetration is incomplete.
A major source of chemo-resistance for many types of cancer comes from glycoprotein transport systems (technically called ABC transporters) that extrude the chemotherapy agent before it has the chance to kill the cell. This is important because chemotherapy is effective only when cells are dividing, and only a fraction of the cell population is dividing at any given time. The longer the chemotherapy remains in the cell, the more likely it will be there at the time of cell division. If extrusion of the chemotherapy drug could be inhibited, chemotherapy should in principle become more effective. Calcium channel blockers, which include commonly used medications for hypertension such as verapamil, have thus been studied for that purpose (11).
Unfortunately, these agents have potent effects on the cardiovascular system, so that dosages sufficiently high to produce clinical benefits usually have not been achievable. However, a recent study (12) did report a substantial clinical benefit for patients with breast cancer with a relatively low dosage (240 mg/day). An earlier randomized trial with advanced lung cancer (13) also demonstrated a significant benefit of verapamil, using a dose of 480 mg/day, both in terms of frequency of tumor regression and survival time. In addition, the combination of verapamil with tamoxifen (which itself blocks the extrusion by a somewhat different mechanism) may possibly increase the clinical benefit (14). In laboratory studies, the calcium channel blockers nicardipine and nimodipine (15, 16) have also been shown to effectively increase chemotherapy effectiveness, and may have direct effects on tumor growth themselves. Quinine derivatives such as quinidine and chloroquine also inhibit the extrusion pump. Among the strongest inhibitors of the extrusion pump is a common drug used in the treatment of alcoholism, Antabuse, also known as disulfiram (17,18). Yet another class of drugs that keep the chemo inside for longer time periods are proton pump inhibitors used for acid reflux (e.g., Prilosec) (19). One approach to blocking the glycoprotein pump without the high toxic doses is to combine several agents together, using lower doses of each individual agent, as combining different agents has been shown to be synergistic in laboratory studies (20).
The most promising clinical results for combatting chemo-resistance has come from the addition of chloroquine, an old anti-malaria drug, to the traditional chemotherapy agent, BCNU. See Chapter 5, Chloroquine section for further details.
Disruption of the blood-brain-barrier (BBB) is also potentially very important and has been extensively investigated. The issue is complicated by the fact that tumor tissue already has a substantially disrupted BBB (which is the basis of using contrast agents to identify the tumor). However, this disruption is incomplete, so any chemotherapy agent that does not cross the intact BBB will not contact all portions of the tumor. Various ways of disrupting the BBB have been studied, but none has been generally successful, primarily because of their systemic side effects. Recently, however, the common erectile dysfunction drugs (Viagra, Levitra, Cialis) have been discovered to disrupt the BBB in laboratory animals. In a rat brain tumor model, the addition of Viagra or Levitra to a common chemotherapy agent, Adriamycin, substantially improved survival time (26).
Optimizing the Schedule of Chemotherapy
The standard schedule for using full-dose Temodar is days 1-5 out of every 28-day cycle. The large phase 3 EORTC-NCIC study (2005) also added daily Temodar during radiation at a lower dosage, followed by the standard five-day schedule after radiation was completed. But there has never been a persuasive rationale for why this standard schedule should be preferred over various alternatives.
In addition to the standard schedule, three other schedules have been studied: (1) a “metronomic” low-dose daily schedule; (2) an alternating week schedule; (3) a “dose- intense” schedule in which Temodar is used on days 1-21 of every 28-day cycle. While it is possible to compare the outcomes of these different studies across different clinical trials, only a few studies have compared the different schedules within the same clinical trial. �In one single-center randomized trial with newly diagnosed patients, the alternating week schedule of 150 mg/m2 on days 1-7 and 15-21 was compared with the metronomic schedule of 50 mg/m2 daily (29). Patients completing 6 cycles of adjuvant Temodar were switched to maintenace therapy with 13-cis retinoic acid (aka Accutane). One-year survival rates were 80% vs. 69%, and two-year survival rates 35% vs. 28%, both favoring the alternating week schedule. However, neither difference was statistically significant. Median survival times for the alternating week and metronomic schedules were 17.1 vs. 15.1 months.
A second very large randomized trial compared the standard 5-day schedule with a dose- intense schedule (75-100 mg/mz2 on days 1-21). The rationale of the dose-intense schedule was that it would better deplete the MGMT enzyme (30). Median PFS favored the dose-dense arm (6.7 months vs. 5.5 months from the time of study randomization, p=0.06), while median overall survival favored the standard schedule (16.6 vs. 14.9 months from randomization). While neither difference was considered statistically significant, the dose-intense schedule had substantially more toxicity and hence cannot be recommended.
In a more recent retrospective study (313), 40 patients undergoing the standard 5-day temozolomide schedule and 30 patients undergoing a metronomic schedule (75 mg/m2) were included in the final analysis. The metronomic temozolomide schedule led to statistically significant increases in both progression-free survival and overall survival, and in both univariate and multivariate analysis. Even more importantly, this study found that the benefit of the metronomic schedule mainly occurs for those patients with EGFR overexpression (EGFR protein expression in over 30% of tumor cells), or EGFR gene amplification. Median overall survival for patients with EGFR overexpression treated with metronomic temozolomide was 34 months, compared to 12 months with standard schedule. EGFR overexpressing patients treated with metronomic temozolomide had highly statistically significantly improved progression-free survival and overall survival compared to all other groups (the other groups being EGFR overexpressing treated with standard schedule, and EGFR non-overexpressing treated with either schedule).
The investigators furthermore analysed tumor tissue samples from patients who underwent repeat resection at the time of recurrence. Interestingly, they found that samples from EGFR overexpressing tumors treated with metronomic temozolomide had significantly fewer cells positive for NF-kB/p65 (a promoter of cell proliferation and survival) compared with untreated tumors from the same patients at the time of diagnosis. No such change was observed between the primary and recurrent EGFR overexpressing tumors from patients treated with the standard schedule. Recurrent EGFR amplified tumors treated with the metronomic schedule showed fewer EGFR amplified cells and weaker EGFR staining at the time of recurrence compared with the primary tumor. No such difference was observed in EGFR amplified tumors treated with �the standard schedule. The authors draw the conclusion that this metronomic schedule impairs survival of EGFR expressing GBM cells more effectively than the standard schedule. These findings will hopefully lead to testing in prospective clinical trials. A major caveat when reviewing this study is that there is no explanation for why some of the patients were selected for the higher dose metronomic schedule rather than the standard schedule and it’s possible that these patients were healthier at baseline and that selection bias contributed to the different outcomes.
The lowest Temodar dose in metronomic chemotherapy reported to date was presented to newly diagnosed glioblastoma patients (44). After completion of standard radiation treatment, continuous daily doses of temozolomide approximately 1/10 of the typically used full dose were used in combination with Vioxx (aka rofecoxib, a discontinued COX-2 inhibitor which was later replaced by celecoxib in studies by this group). Median progression-free survival was 8 months and overall survival for 13 patients was 16 months, with minimal toxicity. A second retrospective study (45) from the same medical group compared the very low-dose schedule (20 mg/m2) with a more typical metronomic dosage (50 mg/meter-squared), although only 17 patients and six patients were included in the former and latter groups. Also included were patients who received only radiation. Median survival was 17 months and 21 months, respectively, for the two metronomic chemotherapy groups vs. 9 months for the radiation-only patients.
Although clinicians will likely resist any alternative to the standard temozolomide schedule for newly diagnosed patients outside of clinical trials, a medium-dose metronomic schedule is worthy of consideration for patients with unmethylated MGMT status, and especially for those patients with unmethylated MGMT status and amplified EGFR. For patients unfit to receive the standard high dose temozolomide schedule, a very low dose metronomic schedule of TMZ may provide some benefit, perhaps through selective toxicity to immune suppressor cells, and in combination with COX-2 inhibition as in the German studies above.
How many cycles of TMZ?
An important question is how long the use of TMZ should be continued. The Stupp clinical trial continued it for only six cycles after radiation, but many patients have continued that protocol for longer period of times.
In what is perhaps the only randomized, prospective trial comparing different numbers of cycles of adjuvant temozolomide, 20 newly diagnosed glioblastoma patients were assigned to six cycles and another 20 patients were assigned to 12 cycles (355). Median progression-free survival outcomes were 12.8 months in the 6-month group and 16.8 months in the 12-month group, which was borderline statistically significant (p=0.069). Median overall survival was 15.4 versus 23.8 months, and achieved statistical significance despite the low numbers of patients included in the trial (p=0.044). A serious limitation of this study is that no information on MGMT status of the patients was collected, and therefore it’s possible that the proportion of patients with MGMT promoter methylated tumors was not equal in the two arms.
A retrospective study done in Canada (51) compared patients who received the standard six cycles of temozolomide with those who had more than six cycles (up to 12) Patients receiving six cycles had a median survival of 16.5 months, while those receiving more than six cycles had a median survival of 24.6 months.
The latest attempts to define the optimal length of monthly temozolomide (TMZ) therapy were published as abstracts for the SNO 2015 annual meeting. In the first of these studies (reference 325, abstract ATCT-08), a large team of investigators retrospectively analyzed data from four large randomized trials with the aim of comparing 6 cycles of monthly TMZ to >6 cycles. Only patients who had completed 6 cycles of TMZ and had not progressed within 28 days of completing cycle 6 were included. Important prognostic factors such as age, performance status, extent of resection and MGMT status were incorporated into the analysis. For these patients, treatment with more than 6 cycles of TMZ was associated with significantly improved progression-free survival [HR=0.77, p=0.03] independently of the examined prognostic factors, and was particularly beneficial for those with methylated MGMT status. Surprisingly, overall survival was not significantly different between the two groups (p=0.99).
In the second abstract (reference 326, abstract ATPS-38), a Japanese group attempted to clarify whether more than 12 cycles of TMZ was beneficial in terms of increased survival. Patients in this study were divided into four groups: a) 12 cycles, b) 24 cycles, c) more than 24 cycles until relapse, and d) beyond 12 cycles (this group includes the b) and c) groups). 12, 14, 12, and 40 patients were included in each of these groups. No significant progression-free survival difference was detected between groups a) and b), implying a lack of benefit of 24 versus 12 cycles. Importantly, patients who were able to continue TMZ treatment for at least 12 cycles (all the patients in this study) had a median progression-free survival of 4.3 years and median overall survival of 6.3 years. This study failed to show a benefit of continuing TMZ cycles beyond 12.
Combining the Standard Treatment with Additional Agents
Few oncologists believe that single-agent treatments are likely to be curative. The issue is finding the optimal combinations, based on toxicities and differences in the mechanisms of actions. Prior to the introduction of temozolomide, the PCV combination of procarbazine, CCNU, and vincristine had been the most widely used combination treatment for glioblastomas, but its use has never been shown to produce a better outcome than treatment with BCNU as a single agent. Nevertheless, there is now a large amount of research studying the effects of combining temozolomide with other therapies, most of which supports the view that such combinations improve treatment outcome, sometimes substantially. A variety of additional therapies are discussed in the following chapters.
Available Treatments
Optune (formerly NovoTTF-100A) by Novocure
| Drug Name | Usefulness Rating | OS_with | OS_without | toxicity_level | toxicity_explanation | |
|---|---|---|---|---|---|---|
| Optune | Optune (Optune Gio® for newer version) | 5 | 20.9 months (Optune plus temozolomide, final EF-14 analysis) | 16 months (control group in EF-14 Trial) | 2 | Most common adverse reaction is skin irritation at the device contact points; no increase in systemic adverse events |
In the spring of 2011, the FDA approved the fourth treatment ever for glioblastoma. Unlike the previous three (gliadel, temozolomide, and Avastin), the new treatment involves no drugs or surgery, but instead uses a “helmet” of electrodes that generates a low level of alternating electrical current. A biotech company called Novocure has developed the device, called Optune, based on experimental findings that electro- magnetic fields disrupt tumor growth by interfering with the mitosis stage of cell division, causing the cancer cells to die instead of proliferating (138). Healthy brain cells rarely divide and thus are unaffected. The treatment involves wearing a collection of electrodes for 18 or more hours per day, which allows the patient to live otherwise normally. This approval in 2011 was the outcome of a randomized phase 3 trial for recurrent glioblastoma, in which Novo-TTF (now called Optune) treatment was equally effective as physician’s choice chemotherapy, but with reduced toxicity and better quality of life (139, 140).
Optune plus chemoradiation, the next standard of care?
EF-14 is a phase 3 randomized clinical trial for newly diagnosed glioblastoma which compared standard of care chemoradiation followed by Optune (NovoTTF) and monthly cycles of Temodar, versus chemoradiation followed by monthly cycles of Temodar alone.
In November 2014, at the annual SNO meeting in Miami Beach, Roger Stupp made a “late-breaking” presentation before a packed audience, describing interim survival outcomes from the EF-14 trial, essentially ushering in what may become the new standard of care for newly diagnosed glioblastoma. This trial is the first major phase 3 trial since the “Stupp protocol” was established in 2005 to report a positive, statistically significant survival benefit for newly diagnosed glioblastoma. In fact, the trial was so successful that it was terminated early and on December 2, Novocure announced that the FDA had approved an investigational device exemption (IDE) supplement allowing all the control patients in the EF-14 trial to begin receiving therapy with Optune tumor treating fields. �The interim results presented in Miami were based on the first 315 patients enrolled in the trial, who had at least 18 months of follow-up. Of these, 105 were randomized into the control arm and 210 were randomized to receive tumor treating fields. Survival and progression-free survival were measured from the time of randomization, which was a median of 3.8 months after diagnosis. Median progression-free survival was 7.1 months in the Optune arm versus 4 months in the control arm (hazard ratio 0.63, with a high degree of statistical significance, p=0.001). Median overall survival from randomization was 19.6 months in the Optune arm versus 16.6 months in the control arm (hazard ratio 0.75, statistically significant, p=0.034). 2-year survival was 43% in the Optune arm versus 29% in the control arm. It must be kept in mind that all these statistics are measured from randomization, roughly 4 months from diagnosis, meaning that median overall survival in the Optune arm approaches 24 months from diagnosis. The statistics above are for the intention-to-treat (ITT) population, which includes all patients randomized, as opposed to the as-treated (per-protocol) population, which excludes patients who did not start their second course of temozolomide or had major protocol violations.
An October 5, 2015 press release announced that the FDA had approved Optune in combination with temozolomide for newly diagnosed glioblastoma, not quite a year after the first survival data from the trial was publicized. This is the first approval of a therapy for newly diagnosed glioblastoma since temozolomide was approved for this indication in March 2005. Two months later, in December 2015, the preliminary results of the EF-14 trial were published in the Journal of the American Medical Association (327). This publication detailed results for the first 315 patients enrolled, the same patients reported upon at the SNO 2015 annual meeting. Additional survival analysis on the per-protocol population (as opposed to the intention-to-treat population) gave an overall survival from randomization of 20.5 months in the Optune group and 15.6 months for the control group (that is, about 24.3 months and 19.3 months from diagnosis) (HR=0.64, p=0.004).
Outcomes for the entire trial population of 695 patients were published for the 2016 SNO conference, with an updated press release from Novocure coming in April 2017. Confirming the results of the interim analysis, median progression-free survival was significantly improved in the Optune group by just under 3 months (6.7 versus 4 months from randomization). Median overall survival from randomization was improved by neatly five months (20.8 versus 16 months). Survival rate at 2 years from randomization was 42.5% in the Optune group versus 30% in the control group. The April 2017 update also reported on 5 year survival rate, which was 13% in the Optune arm versus 5% in the control arm.
As of July 2016, the National Comprehensive Cancer Network (NCCN) had given Optune a 2A listing for newly diagnosed glioblastoma, indicating uniform consensus amongst the NCCN panel that this treatment is appropriate. As the NCCN is known as setting the standard treatment guidelines for cancer in the USA, this formalizes the concept of Optune as part of a new standard of care for newly diagnosed glioblastoma. Although its status as part of a new standard of care may still be disputed by some, Novocure has announced that Optune is now available at over 600 treatment centers in the USA (click here for a list of these US centers), as well as 350 additional institutions internationally, including locations in Germany, Switzerland, Austria, and Japan.
Treatment Categories
Explore the various treatment categories for comprehensive insights and latest developments: CBD
- Repurposed Drugs
- Hormones
- Nutraceuticals
- Antibody-Drug Conjugates and other protein-drug conjugates
- Other Chemotherapy and Cancer Drugs
...
Explore Treatments by Usefulness Rating
Discover treatments that have shown promising results.
Visit our Highly Useful Treatments page to explore treatments rated with a usefulness of 4 or 5.
Hormones
Unlike traditional cancer chemotherapy, which kills cancer cells through directly cytotoxic mechanisms, a different approach may also prove to be effective: manipulation of the body’s balance of circulating hormones to achieve the most unwelcoming environment for the growth of tumors.
Repurposed Drugs
There are a large number of drugs that were developed initially for various different purposes that subsequent laboratory research demonstrated to have significant anti-cancer properties. Given these old drugs have been used for years, have well-defined toxicity profiles, and are generally cheaper due to being off-patent, they offer the possibility of augmenting the benefits of the current standard treatment without significant additional toxicity. However, because their FDA approval is for different purposes, many if not most neuro-oncologists have been reluctant to take advantage of their possible benefits as components of a treatment cocktail. Some of these drugs have been investigated as single agents for brain cancer treatment and some have also been combined with the now standard Stupp protocol.
Over-the-Counter Drugs and Supplements
Nutraceuticals and Herbals
Oncologists routinely warn their patients not to use supplements, usually based on the belief that supplements that are anti-oxidants will interfere with both radiation and chemotherapy. While this issue is extremely complex, my own evaluation of the relevant evidence strongly disagrees with this opinion. Accordingly, I have posted my own analysis of the clinical evidence as an accompanying article on this website. Here I list the supplements that seem most likely to be efficacious, based on extensive laboratory data. Unfortunately, few clinical results are available to corroborate the experimental data, primarily because the supplements cannot be patented; hence there is no financial incentive to develop their clinical usage. The result is that little information is available about the best dosage and bioavailability, which is often a problem. However, a great deal is known about the mechanisms of action of the various supplements, which often overlap those of conventional drug therapy. A detailed consideration of such mechanisms is not possible here, as it would require a great deal of molecular biology. A special issue (2009, Vol. 269, Issue #2) of the journal, Cancer Letters, was devoted to the molecular targets of many of the individual agents to be considered. A more general review is provided in Reference 257.
The list of supplements to be considered is necessarily selective. Undoubtedly, there are numerous other agents that could be useful that are omitted.
Other Chemotherapy and Cancer Drugs
Explore additional chemotherapy and cancer drug treatments:
| Overall Survival without | Overall Survival with | Progression-Free Survival without | Progression-Free Survival with | Usefulness Rating | Usefulness Explanation | toxicity_level | Toxicity Explanation | |
|---|---|---|---|---|---|---|---|---|
| BCNU (Carmustine) and Gliadel (Carmustine Wafers) | Not specified | Gliadel: 13.9 months median survival; Combination with TMZ: Median survival ranges from 17 to 20.7 months | Not specified | Not specified | 4 | Not specified | 4 | The combination of BCNU and Gliadel Wafers in treatment for glioblastoma is assigned a toxicity level of 4, this is relatively high on a scale of 1 to 5. This means that the treatment has serious side effects which may include low blood counts, pulmonary problems, infections, and seizures. Despite these side effects, the improvement in survival rates may make this treatment an important option for many patients. However, managing these side effects could potentially be challenging and may significantly impact the quality of life. It's important to discuss these risks and potential benefits with your healthcare provider. |
| Bevacizumab (Avastin) | Not specified | Not specified | Not specified | Not specified | 3 | Not specified | 4 | The drug Procarbazine is considered quite toxic. This rating is based on the common side effects like hematological toxicity, which refers to potential harm to your blood cells, nausea, and neurological effects such as headache or dizziness. These side effects are relatively common and could significantly affect your day-to-day life. Remember, all treatments come with potential risks, and it's important to discuss these with your doctor. |
| Gleevec (Imatinib) | Not specified | Not applicable; studies focusing on PFS-6 as a primary endpoint | Not specified | PFS-6 value was 53% in a restricted patient population with overexpression of PDGFR | 3 | Not specified | 3 | Gleevec (Imatinib) is at a moderate toxicity level. This is because while it does have side effects such as fluid retention, nausea, muscle cramps, rashes, and fatigue, these are common to most treatments and they vary from patient to patient. Also, it has not been specifically approved for glioma treatment, indicating that it might have unexpected results, slightly increasing the risk factor. However, it has shown some potential benefits in early research, hence the moderate, not high, toxicity rating. |
| Platinum Compounds | Not specified | Not specified | Not specified | Not specified | 3 | Not specified | 4 | The treatment with Platinum Compounds (Cisplatin) is considered relatively high in toxicity due to potential side effects like kidney damage (Nephrotoxicity), hearing loss (ototoxicity), and nervous system damage (neurotoxicity). It's important for patients to discuss these risks with their healthcare provider before starting therapy. A toxicity level of 4 out of 5 means this treatment carries significant risks, but it may be necessary for managing glioblastoma. |
| Procarbazine | Not specified | Not specified | Not specified | Not specified | 3 | Not specified | 4 | The drug Procarbazine is considered quite toxic. This rating is based on the common side effects like hematological toxicity, which refers to potential harm to your blood cells, nausea, and neurological effects such as headache or dizziness. These side effects are relatively common and could significantly affect your day-to-day life. Remember, all treatments come with potential risks, and it's important to discuss these with your doctor. |
CCNU (lomustine)
A report from Germany combined TMZ with CCNU (lomustine), the nitrosourea component of the PCV combination (52). Patients (N=39) received CCNU on day 1 of each 6-week cycle, and TMZ on days 2-6. Eight patients received intensified doses of both drugs, with somewhat better survival results (but with substantially increased toxicity). For present purposes, the results of all patients are aggregated. Median survival time was 23 months, and survival rates were 47%, 26%, 18%, and 16% at 2, 3, 4, and5 years, respectively. Four of the 39 patients had no recurrence at the 5-year mark. Only 23 of the 39 patients were assessable for the status of the MGMT gene. Those with methylated MGMT had a median survival of 34 months, while those with unmethylated MGMT had a median survival of only 12.5 months.
These results, including a 5-year survival rate of 16%, are among the best yet reported, albeit with a relatively small number of patients. But it also should be appreciated that patients who suffered a recurrence received extensive salvage therapy of various types, which may have contributed substantially to survival time. The addition of CCNU to standard therapy for newly diagnosed glioblastoma is currently being tested in a phase 3 trial in Germany.
BCNU (carmustine) and Gliadel (carmustine wafers)
The combination of Temodar with BCNU, the traditional chemotherapy for glioblastomas, has also been studied, but has been complicated by issues of toxicity and the optimal schedule of dose administration for the two drugs. However, a recent published report involving patients with tumors recurring after radiation but no prior chemotherapy failed to show any benefit of combining BCNU with Temodar, compared to Temodar alone, as the PFS-6 for the combination was only 21%, accompanied by considerable toxicity (53).
An important variation in the use of BCNU has been the development of polymer wafers known as gliadel. A number of such wafers are implanted throughout the tumor site at the time of surgery. BCNU then gradually diffuses from the wafers into the surrounding brain. A possible problem with the treatment is that the drug will diffuse only a small distance from the implant sites, and thus fail to contact significant portions of the tumor. However, a phase III clinical trial has demonstrated that survival time for recurrent high- grade gliomas is significantly increased by the gliadel wafers relative to control subjects receiving wafers without BCNU, although the increase in survival time, while
statistically significant, was relatively modest (54). Probably the best estimate of the benefit of gliadel as an initial treatment comes from a randomized clinical trial, conducted in Europe (55), which reported a median survival of 13.9 months for patients receiving gliadel compared to a median survival of 11.6 months for patients implanted with placebo wafers. As with other forms of chemotherapy, larger differences were evident for long-term survival. After a follow-up period of 56 months, 9 of 120 patients who received gliadel were alive, compared to only 2 of 120 of those receiving the
placebo. However, the results were not reported separately for glioblastomas vs. other high-grade gliomas, suggesting that the outcome results would have been more modest for the glioblastoma patients alone.
When gliadel has been combined with the standard TMZ + radiation protocol, survival time seems to be significantly improved, as assessed in three different retrospective clinical studies. In the first, from the Moffitt Cancer Center in Florida (56), the combination produced a median overall survival of 17 months, and a 2-year survival rate of 39%. In a second clinical trial reported by Johns Hopkins, where gliadel was developed (57), 35 patients receiving the combination had a median survival time of 20.7 months and a 2-year survival of 36%. In a third trial conducted at Duke University (58), 36 patients receiving gliadel in addition to the standard TMZ protocol had a median survival of 20.7 months and a 2-year survival of 47%. The Duke cohort also received rotational chemotherapy (which included TMZ) subsequent to radiation. It is important to keep in mind that patients eligible to receive gliadel must have operable tumors, which excludes patients who have received a biopsy only and have a generally poorer prognosis as a result. The effect of this selection bias is difficult to evaluate but it is likely to account for a significant fraction of the improvement in survival time when gliadel +TMZ is compared to TMZ alone.
A major advantage of gliadel is that it avoids the systemic side effects of intravenous BCNU, which can be considerable, not only in terms of low blood counts but also in terms of a significant risk of major pulmonary problems. But gliadel produces its own side effects, including an elevated risk of intracranial infections and seizures. However, the lack of systemic toxicity makes gliadel a candidate for various drug combinations. Especially noteworthy is a recent phase II trial with 50 patients with recurrent tumors that combined gliadel with 06-BG, a drug that depletes the MGMT enzyme involved in repair of chemotherapy-induced damage, but also causes unacceptable bone marrow toxicity when chemotherapy is given systemically. Survival rates at six months, one year and two years were 82%, 47%, and 10%, respectively (59) which seems notably better than the earlier clinical trial with recurrent tumors using gliadel without the 06-BG, in which the corresponding survival rates were 56%, 20%, and 10%. Median survivals were also notably improved by the addition of 06-BG (50.3 weeks versus 28 weeks).
Platinum compounds
An improvement in results relative to those obtained with Temodar alone has also been reported when Temodar has been combined with cisplatin. In a pair of clinical studies performed in Italy (61, 62) with patients with recurrent tumors, the PFS-6 was 34% and 35%. A treatment protocol with newly diagnosed patients that also seems to have produced better results than Temodar as a single agent combined Temodar with both cisplatin and etoposide (VP-16), given through the carotid artery (63). Cisplatin and etoposide were given after surgery and continued for three cycles spaced every 3 weeks apart, followed by the standard protocol of radiation plus low-dose Temodar, then high-dose Temodar on the schedule of days 1-5 of every month. For 15 patients studied, median survival was 25 months.
Procarbazine
Temodar has also been combined with procarbazine (64). While the report of that study did not include the PFS-6 statistic, it did report an unusually high percentage of tumor regressions, suggesting that this combination might be effective.
Bevacizumab (Avastin)
The most notable development in drug combinations has been the addition of the anti- angiogenic drug, Avastin (also known as bevacizumab), to the standard Stupp protocol. As will be discussed later, Avastin has FDA approval for the treatment of glioblastomas that have recurred or progressed after initial treatment. Several clinical trials have now investigated its combination with the gold standard Temodar protocol.
Recently, there have been two large randomized phase III clinical trials comparing
the Stupp protocol and the Stupp protocol + Avastin, for newly diagnosed patients. In the first of these (70), known as the AVAglio trial, median PFS was 10.6 months for those receiving Avastin versus 6.2 months for those receiving only the Stupp protocol, a statistically significant difference. However, median overall survival was not different (16.8 months vs. 16.7 months). It should be noted that patients in the control group typically received Avastin after tumor progression occurred, so that the comparison was really between Avastin given early versus Avastin given only after recurrence. Additional results were that 72% of the Avastin group was alive at one year, compared to 66% of the control group, while two year survival was 34% vs. 30%.
In the second of these large trials (71), conducted by the RTOG consortium, the design was essentially similar to the AVAglio trial, as were the results. Median PFS was 10 months for those receiving Avastin vs. 7.3 months for the control group (again statistically significant), while median overall survival was 15.7 months for the Avastin group compared to 16.1 months for the control, a nonsignificant difference.
The best interpretation of these results is that patients have a longer time without tumor progression, and presumably a better quality of life, when Avastin is used as part of the initial treatment. However, there is no benefit for overall survival, when compared to withholding Avastin until recurrence is detected. An additional feature of the results, not emphasized by the authors of the reports, is that the overall survival times were not notably better, and in many cases worse, than those obtained when the Stupp protocol is combined with various other treatment agents.
EGFR inhibitors: Iressa, Tarceva, and Erbitux (gefitinib, erlotinib, and cetuximab)
These three drugs, which have FDA approval for several different types of cancer, have the common feature that they target a growth-signaling channel known as the epidermal growth factor. Overexpression or mutation of EGF receptors is involved in the growth many different kinds of cancer, including more than half of glioblastomas. In general, use of these drugs as single agents has produced disappointing results, although occasional long-term survivors have occurred. More promising results have occurred when EGFR inhibitors have been used in combination with the Stupp protocol.
When Tarceva has been added to the standard Temodar protocol for newly diagnosed patients, median survival was 15.3 months (N=97) in one study (72) and 19.3 months (N=65) in a second study (73). The results of the second study were compared to two previous phase II trials involving a similar patient population, in which Temodar was combined with either thalidomide or accutane. Median survival for those trials was 14.1 months.
The moderately positive results of the just described trial are in conflict with a very similar trial (N=27) conducted at the Cleveland Clinic (74). In that trial median survival was only 8.6 months, notably worse than the outcomes obtained when temodar has been used without tarceva. How the conflicting results can be reconciled is unclear. Erbitux (also known as cetuximab) is a monoclonal antibody, which differs from Iressa and Tarceva, which are small molecules, Because monoclonal antibodies are not believed to cross the blood-brain barrier, the natural expectation is that Erbitux would be ineffective against brain tumors. As a single agent, this seems to be true, as PFS-6 was only 10% for patients with recurrent high-grade gliomas (75). But when Erbitux was added during the radiation phase of the standard temozolomide protocol for 17 newly diagnosed patients (76), 87% of patients were alive at the end of one year and 37% were progression free. The median survival time had not been reached at the time of the report (an abstract at a meeting). It is possibly important to note that some investigators believe that radiation temporarily disrupts the blood-brain-barrier, which would allow a monoclonal antibody such as erbitux to reach the tumor.
An important development for identifying patients likely to respond to Tarceva has come from a study (77) of glioma patients whose tumor pathologies were also assessed for their levels of a second protein called PKB/AKT. This is a signaling channel that results from inactivation of the PTEN gene, a tumor suppressor gene commonly mutated in glioblastomas. None of the tumors with high levels of PKB/AKT responded to treatment with Tarceva, whereas 8 of 18 tumors with low levels did respond to the treatment. A refinement of this approach tested for three different proteins: expression of PTEN, expression of EGFR, and of a mutation of the EGFR protein known as EGFR variant III (78). The level of EGFR was not related to clinical outcome, whereas the co-expression of EGFR variant III and PTEN strongly predicted clinical outcome.
Because the inhibition of PKB/AKT should plausibly increase the effectiveness of EGFR inhibitors, a treatment strategy now being tested is the combination of EGFR inhibitors with rapamycin (trade name rapamune, generic name sirolimus), an existing drug used for organ transplants to suppress the immune system and prevent organ rejection, but which also inhibits mTOR complex 1, a tumor growth promoter downstream of AKT. A phase I trial (79) combined Iressa with rapamycin for 34 patients (25 GBM) with recurrent tumors; two patients had a partial tumor regression and 13 patients achieved stable disease. PFS-6 was 24%. A second clinical trial (80) with 28 heavily pretreated patients with low performance status (median Karnofsky score of 60) received either Iressa or Tarceva in combination with rapamycin, with the result that 19% of patients had tumor regression while 50% had stable disease, with a PFS-6 value of 25%. Yet a third clinical trial (81) that combined tarceva and sirolimus for recurrent GBM had much worse results, with PFS-6 value of only 3%.
The foregoing results of the use of EGFR inhibitors for GBM treatment range from moderately positive to minimal efficacy. The reasons for this variability are not obvious, although treatment efficacy is likely dependent on numerous genetic markers. Thus, without a genetic analysis of individual tumors, it is hard to see a basis for recommending their use. �One recent paper (83) of potential major importance has noted that tumors may not respond to anti-EGFR drugs because of activation of the gene for a second growth factor known as the insulin-like growth factor receptor I (IGF1R). IGF1R has also been implicated as a source of resistance to tamoxifen and various other treatment agents. It is noteworthy, therefore, that two of the supplements to be discussed, silibinin and lycopene, are known to inhibit IGF-I. This suggests that silibinin and lycopene might substantially increase the effectiveness of any treatment that relies on EGFR inhibition. Metformin, a widely used diabetes drug, is also known to reduce the level of IGF-1, currently is under investigation as a treatment for several different kinds of cancer.
An important issue is how the effectiveness of EGFR inhibitors are related to the findings discussed earlier that metronomic schedules of Temodar produce a large survival improvement for GBMs that have EGFR overexpression. All of the clinical trials discussed in this section used the standard Temodar schedule, so it is unclear whether a metronomic schedule might produce different outcomes.
Gleevec (imatinib)
Gleevec (also known as imatinib), a small molecule which targets a specific gene involved in the growth of a form of leukemia, received a great deal of publicity because of its unprecedented effectiveness. As will be discussed later, this general strategy of identifying the growth signals for tumor growth and then targeting those signals, or their receptors, is one of the major new areas in cancer research. Such growth signaling channels often are involved in several different types of cancer. Although Gleevec was developed specifically for chronic myelogenous leukemia, it also has been shown to inhibit a more general type of growth signal, platelet-derived growth factor (PDGF), which is also involved in the growth of gliomas and other forms of cancer (e.g., small- cell lung cancer). Laboratory research has supported the importance of this similarity in that gleevec has been shown to strongly inhibit glioma growth, with the result that there now have been a number of studies reporting its use with high-grade gliomas.
The generally disappointing results using gleevec for brain tumors may have occurred
for several different reasons. It may not readily cross the blood-brain-barrier, and it may engender different mechanisms of resistance than other treatment agents. In the study of gleevec for leukemia, for example, high levels of autophagy have been observed, which can be inhibited by the concurrent use of chloroquine or other autophagy inhibitors.
An important variation in the use of gleevec was to restrict its usage to patients with recurrent tumors who tested positive for overexpression of the platelet-derived growth factor receptor (90). PDGFR is overexpressed in 50-65% of tumors, especially tumors labeled secondary glioblastomas, which are believed to have evolved from lower-grade tumors (in contrast to de novo glioblastomas that occur without such evolution). For this restricted patient population, the PFS-6 value was 53%.
Treatments for Recurrent Glioblastoma
While Temodar is now the drug of choice for the initial treatment of glioblastoma, the majority of patients will receive minimal benefit. Patients who have failed the standard treatment protocol often proceed to other chemotherapy drugs. These include the nitrosoureas, BCNU and CCNU (and ACNU in Europe and Japan), and also the platinum drugs, and irinotecan, a drug developed for colon cancer known also known as CPT-11.
Promising new Treatments
Antibody-Drug Conjugates and other protein-drug conjugates
Investigate the cutting-edge Antibody-Drug Conjugates and other protein-drug conjugates being developed:
| Overall Survival without | Overall Survival with | Progression-Free Survival without | Progression-Free Survival with | Usefulness Rating | Usefulness Explanation | toxicity_level | Toxicity Explanation | |
|---|---|---|---|---|---|---|---|---|
| ABT-414 | Not specified | Not reached at a median follow-up of 5.8 months | Not specified | 6.1 months for all patients, 5.9 months for EGFR amplified patients | 2 | Not specified | 4 | The drug ABT-414 is in phase 1 of its clinical trials. It demonstrates a tendency towards eye toxicities, especially causing blurred vision. This is an indication of potentially high toxicity. However, due to small sample size and other variables in the study, the evaluations should be taken with caution. It is advised to expect a higher level of toxicity until tested further in next clinical trial phases. |
| MDNA55 | Not specified | Not specified in the provided text | Not specified | Not specified in the provided text | 3 | Not specified | 2.5 | The treatment, MDNA55, is in its early phase of trials, meaning that its potential side effects are still being evaluated. Currently, it's not fully approved by the FDA and exact toxicity is not specified. However, MDNA55 is designed to target cells common in tumor tissue, creating a high potential for effectiveness with fewer harmful effects on healthy tissue. It has shown significant positive response rates, suggesting a manageable toxicity profile. Nevertheless, every treatment carries some risk, and potential side effects might still be discovered. The toxicity rating of 2.5 out of 5 indicates a moderate risk of toxic side effects at this point in time. |
Immunological Approaches
Because cancer cells have a genetic structure different from normal cells they generate foreign proteins that in principle should be detected by the immune system and evoke the same type of immune reaction as any foreign virus or bacteria. This basic fact suggests that augmenting one's immune system might be an effective approach to cancer treatment. Such an approach has an immediate appeal because it is surely preferable to reinforce the immune system than to poison the entire body in the hope the cancer cells will be killed before the body is depleted of vital resources. However attractive this philosophy may be, translating it into an effective cancer treatment has proven to be extraordinarily difficult. Contrary to general belief, immunological treatments are not �benign to implement. Interferon treatment has very definite debilitating effects, as do cytokines such as interleukin-2 and tumor necrosis factor, because their modus operandi are essentially to create an inflammatory immune reaction not unlike a severe allergic reaction. When this inflammatory process is too severe, it can in fact be fatal.
Vaccines
The holy grail of immunological approaches to cancer treatment is the development of effective vaccines. In principle this should be possible because of the differences in the protein structure of cancer cells and normal cells. But, two general problems must be overcome. The first is that different individuals have tumors with different collections of antigens (proteins), so that generic vaccines are unlikely to be effective; thus patient- specific vaccines are required. The second problem is that the immune system is not an efficient detector of the tumor's foreign antigens. In part this is due to the tumor secreting enzymes that in effect provide a protective cloak preventing such detection. The larger the tumor the stronger is its defense mechanisms to counteract immune-system detection. This is one reason that most vaccines work best when there is a minimum of tumor burden.
Personalized vaccines
DCVax and other lysate-pulsed dendritic cell vaccines
Tumor-associated antigen vaccines
based on this book: Treatment Options for GBM - 2017 By Ben Williams
If you want to add treatments, you can use this GPT to help research and format the results